This course supplies skills for CNAs and HHAs. These professionals work in many places, like healthcare facilities and private homes. Each setting has unique safety challenges. So, knowing safety protocols is key.
OSHA standards are key to workplace safety. Using Personal Protective Equipment (PPE) properly is a vital part of this. Workers must understand their rights. They have the right to a safe workplace. They can also report hazards without fear.
Hazardous chemicals are common in healthcare and home settings. Reading Safety Data Sheets (SDSs) helps workers understand the risks of chemicals. Proper storage, handling, and disposal of hazardous materials are essential to avoid accidents. Spill response plans must be clear and practiced to limit the impact of chemical spills.
Exposure to hazardous chemicals can lead to serious health issues. Knowing how to decontaminate and use emergency eye wash and shower stations is key. This helps reduce exposure effects. Monitoring exposure and knowing permissible exposure limits (PELs) helps keep the workplace safe.
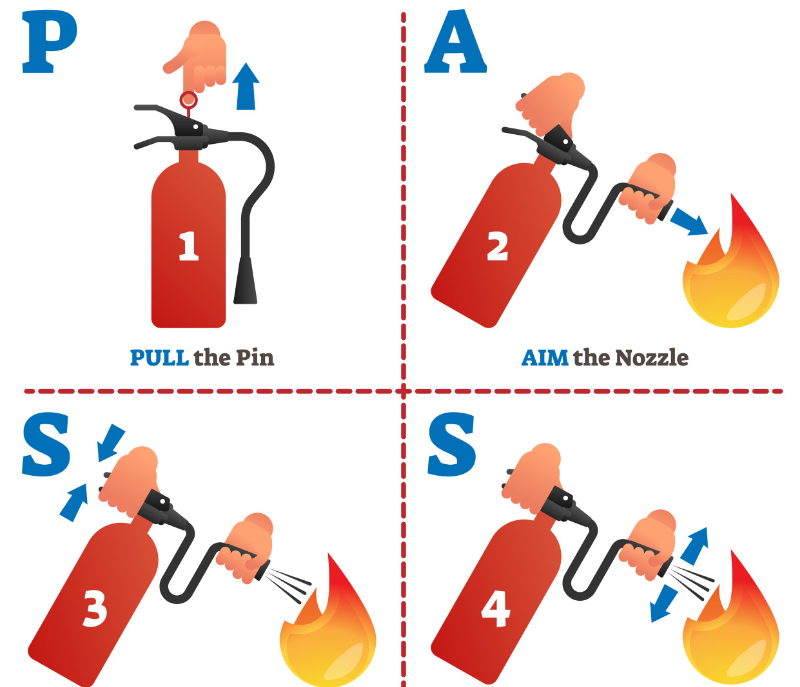
Fire safety is a serious risk in healthcare. Flammable materials and electrical equipment can cause fires. It’s important to know fire types, their causes, and how to prevent them. Training on fire extinguishers is key. This training teaches workers the PASS method for small fires. Fire alarms, smoke detectors, and sprinklers send early alerts and help fight fires. Understanding how these systems work allows for quick evacuations. Oxygen safety is critical in areas with oxygen therapy. Knowing the risks in oxygen-rich spaces is essential. Safe handling of oxygen cylinders is a must.
Practicing evacuation procedures is crucial. This includes both horizontal and vertical evacuations. Focusing on patient movement and using aids ensures safety during emergencies. Fire doors and walls help contain smoke and flames. Knowing their functions and ratings is important.
Healthcare workers face many safety risks. These include reproductive, respiratory, and skin hazards. Knowing these risks and using PPE is essential for protection. Also, managing stress and preventing violence is important for workplace safety.
Communicable diseases, like bloodborne pathogens, are serious threats to healthcare workers. It's important to adhere to exposure control plans and post-exposure steps. Doing this helps prevent infections. The unique risks of in-home healthcare need careful assessment and planning.
Training courses establish safe work practices. Ongoing education and adherence to safety protocols are key. They help protect healthcare workers and patients alike. By prioritizing safety, healthcare workers can lower risks and deliver quality care.