The main goal is to prevent asthma attacks and minimize risks. Once triggers have been identified, a plan can be developed with the patient to avoid them and how to handle an attack when it occurs. The resident’s care plan should include how to avoid the triggers for that person. Help the resident avoid triggers and fix or report anything in the environment that may be a trigger. An example might be the exhaust from trucks running by the facility getting into the resident’s room, triggering asthma attacks for the patient. Report this to the nurse. That resident needs to be moved. Residents with asthma should not participate in animal therapy if they are allergic to animals.
The resident should be able to recognize the signs and symptoms of an attack. They should know how to use the medication provided, what triggers to avoid, and when to seek medical attention (CDC, 2023). Avoiding triggers may be a problem if the resident has dementia or becomes confused.
Anyone can be subjected to an asthma attack at any age and for many reasons. We do not always know the reason. It may be a family trait. It may be a response to allergic reactions. It may be due to mold or dampness. As a few examples, asthma can occur from dust mites, secondhand tobacco smoke, and air pollution (CDC, 2018). A lung infection may also lead to asthma (CDC, 2023). Adult asthma can develop in females during childbearing years and may occur during or after pregnancy. Adults tend to have asthma for life once they develop the condition.
Allergies to animals or plants may trigger an attack. Exercise-induced asthma occurs after strenuous activity.Occupational asthma is caused by inhaling fumes, gases, or dust while at work. A person with allergies is more likely to develop occupational asthma. Nocturnal or nighttime asthma can also occur. This type of asthma is worse at night. It can be caused by the position while sleeping, hormones, circadian rhythms, night air, air conditioning, gastroesophageal reflux disorder, or allergy exposure. Other issues that can impact the development of asthma include obesity and coexisting diseases like chronic obstructive pulmonary disease (COPD) (CDC, 2023).
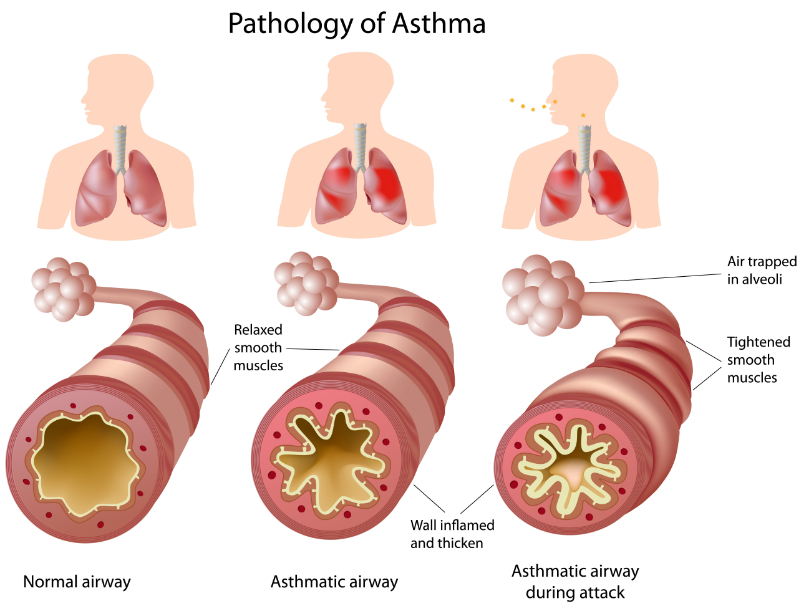
The patient usually has long-term medication, such as an inhaler, to reduce inflammation, which is taken daily. However, they can also use quick-relief inhalers during asthma attacks. The quick-relief medication relaxes the muscles of the airway, relieving symptoms. The patient should also know when to contact emergency services for needed help.
During an asthma attack, the patient should sit down, preferably in a semi-fowler position to help with breathing. The patient should try to relax as much as possible and breathe from their diaphragm. Remember that hypoxia can occur easily. Any signs of lips or nails turning blue are cyanosis and mean that they need medical attention. If the patient has an inhaler, they should use it to try to gain respiratory control (Mayo Clinic, 2022). Remember, the goal is to relieve hypoxia and airway obstruction or inflammation as soon as possible.
Help the patient to remain calm and reassure them that you are staying with them until they feel better. Explain to the patient that anxiety and agitation will be better if they can try to relax their breathing. If possible, monitor vital signs. Breathing heavily during an attack can drain energy from the patient and cause dehydration. Once the attack has passed, the patient may be dehydrated. Offer fluids to help maintain their fluid balance.
A patient with asthma may have a limited quality of life. Several things cause a poor quality of life. First is the patient’s inability to sleep. Lack of sleep can be an issue for a child who has to get up and go to school or those who must be to work on time. Physical activity can be limited as well, putting the patient at a greater risk of developing medical issues, including obesity and depression (Mayo Clinic, 2022).