A 38-week gestation infant, Cindie, was born with slow respirations.
Pregnancy and labor were all normal, with no risk factors.
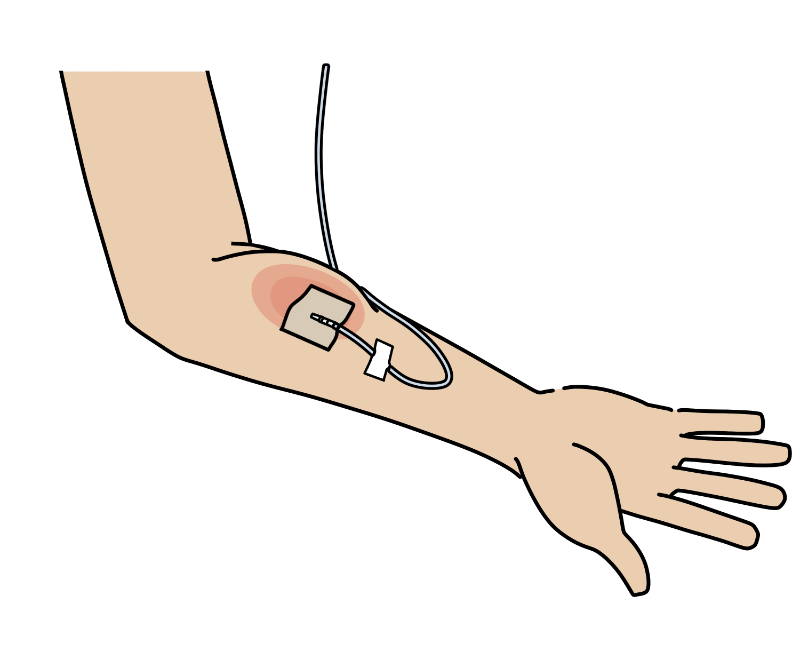
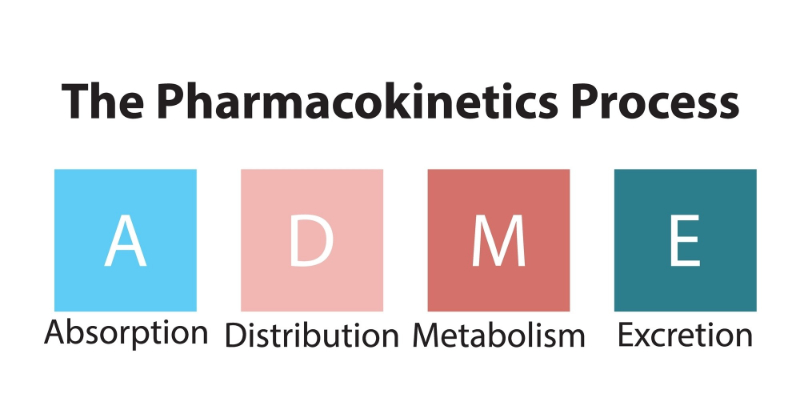
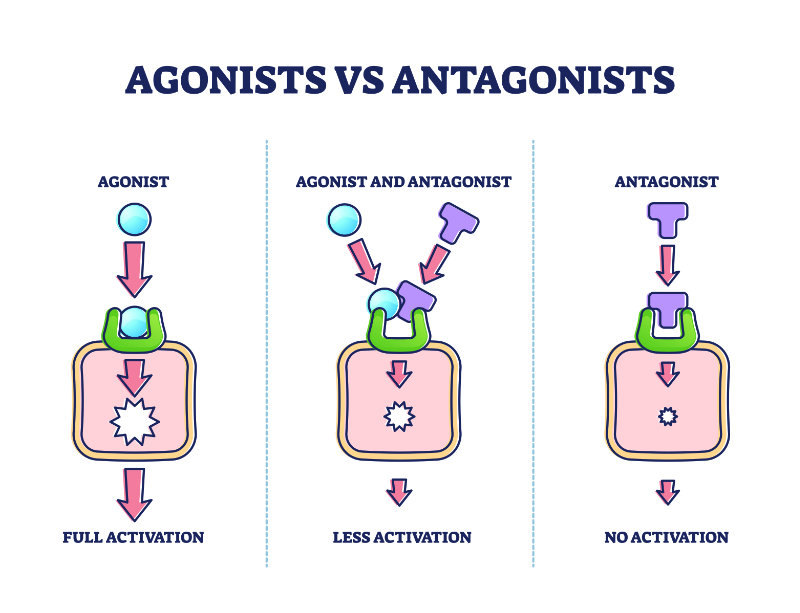
During labor, Cindie’s mother had received meperidine, a narcotic with a half-life of 2.5-4.0 hours in adults. Meperidine also has a half-life of 12-39 hours in neonates. Cindie’s mother had received the medication at 5 cm of dilation, but labor progressed quickly, and she delivered within 2 hours of receiving it. The nurse, along with the physician, began the initial steps of infant resuscitation. The physician also asked for naloxone. Shortly after administering the drug, the infant's condition began to deteriorate further (Franklin, 2003).
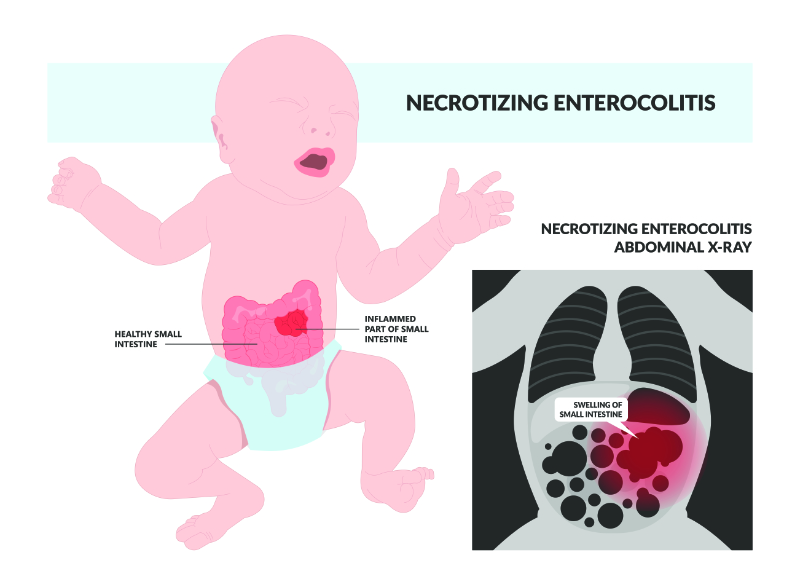
Because of the worsening of the neonate so close to the administration of the naloxone, the physician checked the drug's packaging. The physician found that the syringe had been filled with digoxin, a cardiac drug instead of naloxone. The drugs are both made by the same manufacturer and the packages were very similar. The electrocardiogram revealed a bi-directional ventricular tachycardia, an arrhythmia consistent with digoxin toxicity (Franklin, 2003).
Approximately one hour later, Cindie passed. A post-mortem digoxin level was drawn and found to be 17 ng/ml. The therapeutic range is 0.8 to 2 ng/ml (Franklin, 2003).
In this case, both drugs were made by the same manufacturer and presented in similar packaging. Both of these medications would be stocked on most neonatal units, and the doses to be given are very similar.
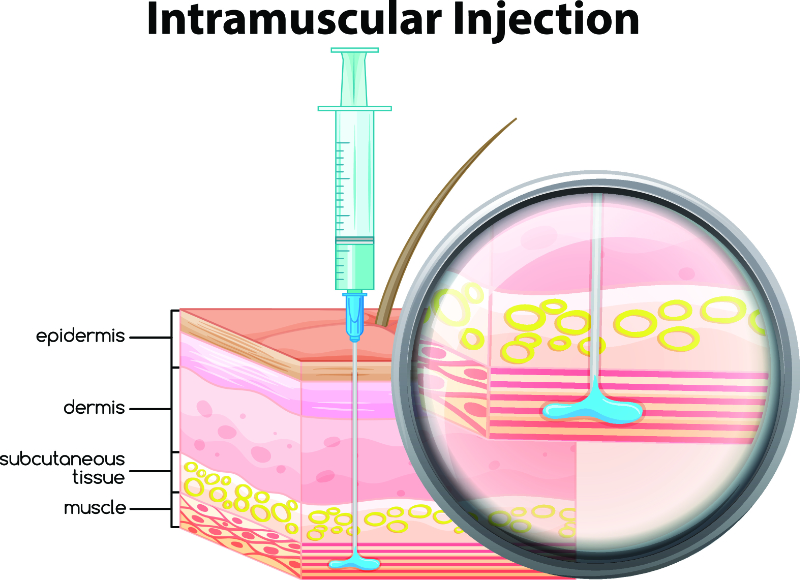
The IV dose of naloxone that is recommended for use in newborn babies is:
10 mcg/kg every 2-3 minutes
The IV a digoxin loading dose is:
10 mcg/kg to 17.5 mcg/kg, depending on age
If the individual who administered the drug confused naloxone with Lanoxin because of the brand name for naloxone or because the name was misread, there would be few signs to suggest that the wrong medication had been chosen until after it had been administered (Franklin, 2003).
Administration errors in hospitals have been cited to be roughly about 3%-8% of doses in the United Kingdom (UK) and about 0.6%-14.6% in the United States, excluding wrong time errors (Franklin, 2003). While methods and definitions may vary, it is clear that administration errors are not uncommon. Fortunately, most errors in medication administration do not result in outcomes as tragic as in this case (Franklin, 2003).
It is important to know that errors in drug administration do occur. Packaging and look-alike/sound-alike drugs are known to be contributing factors of these errors. Risk assessments should be completed and should assess look-alike and sound-alike products and consider how they are stored. Good communication between medical and nursing staff is known to help to prevent medical errors. Anytime an error does occur, there should be a root cause analysis to determine if there is room to make process improvements in how the medication is used and/or given. Patients and their families desire and deserve disclosure of errors and information on how similar errors will be prevented in the future (Franklin, 2003).