The treatment of allergic reactions begins with avoidance of triggering stimuli and then medical treatment after exposure to an allergen. Removal of certain items that can collect allergen material (soft pillows, stuffed animals, etc.), frequent washing/cleaning to remove allergens from the environment (and use of HEPA filters) and removal of irritants such as perfumes, smoke, odors, etc. can all help to avoid allergic reaction. Severe reactions should not be attempted to be cared for at home (Merck, 2007; Haith, 2005).
There are several medications that are used to block the action of allergenic mediators (called antagonistic drugs) to prevent the activation of cells and to prevent them from degranulating. Included in these are antihistamines, corticosteroids, epinephrine, theophylline, and cromolyn sodium. Anti-leukotrienes are also used. Anti-cholinergics, decongestants, mast cell stabilizers, and others may help to prevent the movement of eosinophils in response to allergens. These only treat the acute phases of an allergic reaction, and are not for the chronic treatment of allergy (Wikipedia, 2008).
Antihistamines are used to block histamine receptors in the body. Histamine-1 (H1) blockers are widely used for allergic disorders, histamine-2 (H2) blockers are most effective the in gastrointestinal tract for acid suppression and are not usually used in the treatment of atopic disorders. H1 blockers are most effective in the treatment of atopic disorders and are less effective in treating bronchoconstriction (in asthma) and vasodilation. Antihistamines can be used intranasally and ocularly as well. The most common side effect from oral antihistamines is drowsiness (Merck, 2007; Haith, 2005).
Mast cell stabilizers can be used to block the release of mediators from mast cells and their subsequent effects. These are usually used when antihistamines and corticosteroids are not available or are contraindicated (Merck, 2007).
Antiinflammatories are used to treat symptoms of allergic reaction due to swelling. NSAIDs are not effective enough to do this, and thus, corticosteroids are the drugs of choice. Corticosteroids reverse the effect of systemic mediators. Nasal corticosteroids are most often prescribed and have few side effects as compared to corticosteroids taken orally or via injection (Merck, 2007; Haith, 2005).
Leukotriene modifiers are used in the treatment of asthma and seasonal allergic rhinitis to prevent the side effects from leukotriene production by the body (Merck, 2007).
Anti-IgE antibody is used for more severe cases of asthma that do not respond to other treatments and may also be helpful in cases of rhinitis that are refractory to other treatments (Merck, 2007).
Decongestants can be given to reduce sinus drainage and relieve nasal congestion and swelling, and sinus pain (Haith, 2005).
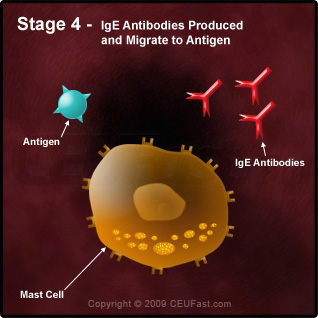
Treatment by immunotherapy is based on the theory of hyposensitization/desensitization via injection of the allergen to the patient. This does not treat the symptoms of an allergic reaction, but alters the immune response to prevent further reactions by increasing IgG production which in turn blocks excessive IgE production. This form of treatment is indicated when the patient cannot avoid allergen exposure and medical treatment is not otherwise available. This is done by giving an injection of the allergen monthly. The dose of the allergen is increased until a maximum tolerated concentration is reached, meanwhile observing the patient to ensure no serious reaction takes place. This maximum dose is then given every 4 to 6 weeks year round. This can be done for most allergens including pollen, dust, mold, and insect venom. It can be done for animal dander in those who cannot avoid exposure and for certain antibiotics such as penicillin. Food desensitization is not performed (Merck, 2007; Haith, 2005; Wikipedia, 2008). A second type of immunotherapy is performed in which monoclonal anti-IgE antibodies are injected into the bloodstream which bind to free IgE and destroys them. (It does not affect IgE that are already bound to the FcεRI receptor-if it did, it would signal a response instead.) Sublingual immunotherapy is a third form which is orally administered and uses oral immune tolerance to antigens such as foods and resident bacteria. Oral tolerance refers to specific suppression of cellular and/or humoral immune reactivity to an antigen by administration of the antigen orally (Wikipedia, 2008).
In the event that a patient has an anaphylactic reaction, evaluation in the emergency department is performed on the basis of stabilizing the patient by monitoring blood pressure, respiratory sufficiency, history of what possibly caused the reaction, and an IV line is often placed in case of further/continued emergency. Epinephrine is given in anaphylaxis and works by dilating the bronchioles (bronchodilator) and constricts blood vessels (to increase blood pressure) (Haith, 2005).