Chances are, you will have several patients with arthritis. This chronic disease forces them to change how they manage their daily lives. There are several things that you can do to help the patients. Remember that some days will be better than others for them. One day, they may be able to do several activities independently; other days, they may need a lot of help. When the patient has flare-ups that include inflammation, it will be important to check to make sure shoes or slippers fit correctly. It is also important to remind your patient to change positions frequently. This includes their neck, hands, arms, hips, and feet. Encouraging them to stretch often can help decrease the stiffness they feel in their joints. Remind the patient to use their strongest joints first and encourage them to sit in chairs with arms so they can push up when rising. Ensure the patient maintains a good balance between rest and activity. The patient may have splints or other devices to help them. Make sure you know how to use the splints and devices properly. Talk to your patient about proper posture since it can prevent additional joint damage. Encourage them to use assistive devices whenever possible.
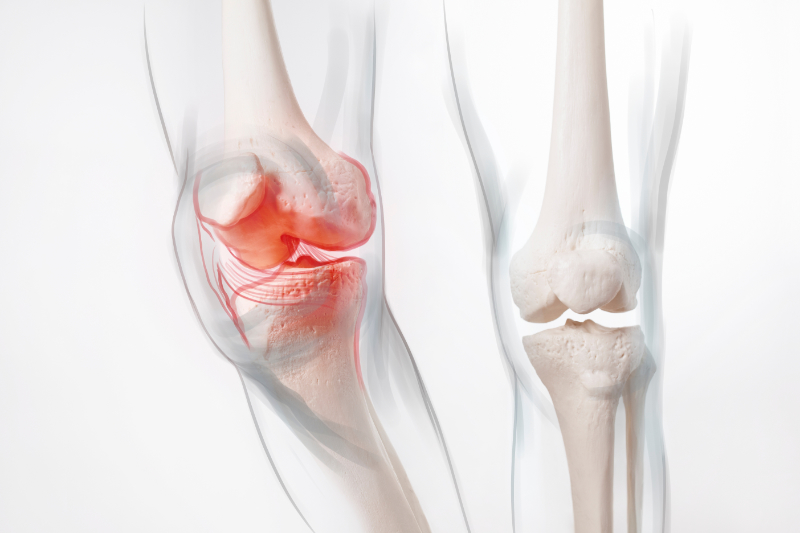
The patient may have or be at high risk for muscle loss and contractures due to a lack of movement. Be sure to follow any range-of-motion exercise care plans. Do not over-extend a joint. With arthritis, the ability to bend a joint may be much less than normal. Follow the instructions carefully for each planned exercise. If you are unsure about any exercise or how it is performed, ask the nurse before proceeding. Be slow and gentle. Do not make the joint move past any resistance you feel or pain the patient shows. Support each joint by placing one hand above and the other below the joint. Encourage the patients to assist if they can. Be sure to observe if the patient is in pain or becomes uncomfortable. If you need to transfer the patient, use transfer assistive devices to make the move easier for you and the patient.
There are several areas to consider when working with a patient with arthritis. Not only does physical pain need to be addressed, but psychological issues, family issues, and societal issues may also need to be treated. The patient may feel fearful, anxious, or depressed at losing their independence and the ability to care for themselves. They may want information on self-care. The decrease in activity may lead to losing a job and financial stability. Changes in family roles and relationships may also concern the patient. Each area will need to be addressed, and care will be applied to help the patient cope both physically and emotionally. Emotional Support helps the patient to stay positive.
Here are some other ways that can be used to relieve pain and help the patient with daily activities. These treatments are delegated by nurses and detailed in the care plan (Sorrentino & Remmert, 2021). Medication may be used to help control pain and inflammation. Helping the patient with weight control through diet and passive exercise can lessen the strain on the joint and prevent further injury. Be sure to follow the care plan about diet and exercise.
Non-pharmacological pain control may include heat and cold packs, distraction techniques, or relaxation programs—for example, music or guided imagery. Heat increases blood flow and circulation to fight infection and take away fluids from swollen areas. Cold reduces blood flow, which slows down swelling and can the numbness reduce pain. Chemical ice and heat packs are activated by squishing the pack, creating a chemical reaction. There are also assorted hot and cold packs that are manually filled with ice or hot water. Protect the skin from direct contact with heat or cold packs. Padding must be used. There are also devices for soaking in hot or cold water (Sorrentino & Remmert, 2021). Make sure you know how to use the products.
Exercise increases flexibility, decreases pain, and helps improve blood flow. It can also help if weight control is problematic and can benefit mental well-being. For patients with arthritis, over-exercising can increase stress and pain. The swelling and pain may not be noticed for hours (Sorrentino & Remmert, 2021). Exercise will be determined in advance and noted on the care plan.
The patient with arthritis is at a greater risk for falls. Helping them with their activities of daily living may include using toilet seat risers, chairs with higher seats and arm sets, and using assistance devices to move positions or to walk(Sorrentino & Remmert, 2021). All of these actions help prevent falls.
Rest is important for the patient with arthritis, especially after exercising or increasing movement. Make sure the patient uses good body mechanics and posture, as well as canes or walkers for support. There should be a good balance between activity and rest.
Helping the family cope may also include changing family roles and responsibilities. Encouraging and praising patients when they do things independently can help them maintain a positive outlook (Sorrentino & Remmert, 2021).
Encourage patients to brush their teeth at least twice daily. An electric toothbrush may be helpful if the patient fatigues easily while holding a brush, and an oral rinse may also help with dry mouth. Devices to make the toothbrush handle larger and more accessible to hold are also available if the hands are affected by arthritis.
When dressing, it may be helpful to get shoes with Velcro straps instead of ties or use a long-handled shoehorn to put on shoes. If zippers are difficult to grab, use a ribbon tied to the zipper for the patient to grab instead. A long grabber can also help pick up items from the floor or lower areas. Chairs or stools in the kitchen and bathroom can help with fatigue as well (Sorrentino & Remmert, 2021).