Be sure there is a clear understanding of all orders, including positioning, monitoring and limiting fluid intake, diet restriction, weight monitoring, vital signs schedule, and activity. The CNA may be asked to strain the urine for particles, help with urination, or collect urine samples.
Knowing how to limit fluid is also very important. Most adults take in 2 1/2 to 3 quarts of fluid a day (National Kidney Foundation, 2024b). This would be approximately 600 to 800 mL of fluid in an eight-hour shift. However, there is typically more fluid intake in the morning. Be sure to observe for edema and dehydration. Output of fluid consists of urine, sweat, lung exhalation, and bowel movements. So, include diarrhea, vomiting, or blood loss as output. A normal adult loses approximately 2 1/2 quarts a day of fluid (Sorrentino & Remmert, 2021).
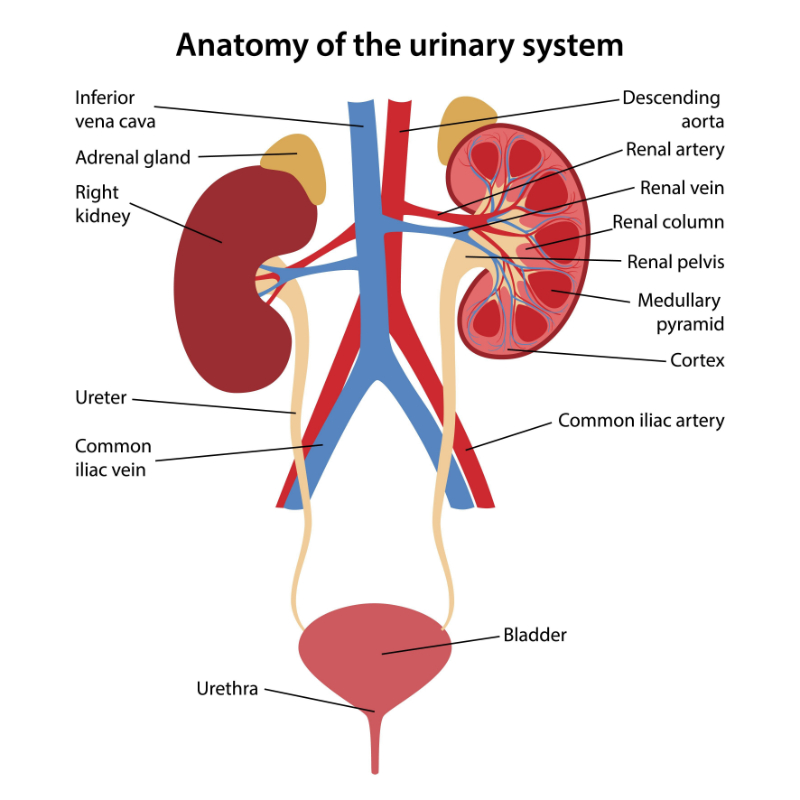
There may be an order to monitor and record intake and output for the patient. Measuring is typically done in liters or milliliters. The CNA must know how many ounces are in milliliters. For example, eight ounces equals 240 mL, sixteen ounces equals 480 mL, and four ounces equals 120 mL. If the patient has an IV or gastric tube, it is recorded separately. If the patient is incontinent, weighing the briefs or sheets can give an estimated output. If the output of urine falls below 30 mL in an hour, it is important to notify the nurse immediately because it may be a sign of dehydration or renal failure(Sorrentino & Remmert, 2021).
Vital signs should be taken daily. Orthostatic blood pressure may be ordered. This means the blood pressure is taken in supine, sitting, and standing positions. The reason for using different positions is to see if the blood pressure drops when the position is changed. A big drop when a position is changed indicates that the circulatory system is not working correctly.
Daily weights are important to measure whether the patient is retaining fluid. For accuracy, weigh the patient at the same time every day using the same scales. If the weight increases or decreases by a certain amount, be sure to inform the nurse immediately. (National Kidney Foundation, 2024b). The amount may be different for different people. A weight change of ten pounds in one day is a common amount to report to the nurse.
If the patient is bedridden, prevention of pressure ulcers and range of motion may be ordered. Measures to prevent itching, such as bath oils, lotions, or creams, can be used on dry skin. Frequent oral hygiene should also be performed since dry mouth can happen. Providing frequent rest periods and emotional support is also important.
Additionally, foods should be low in protein, potassium, and sodium. (National Kidney Foundation, 2024b). Protein can build up and cause more waste in the bloodstream. Sources of protein are typically from animals and legumes. Examples are eggs, beans, fish, and chicken. Sodium can cause fluid buildup and should be monitored carefully.
Sources of sodium are salt, tenderizers, steak sauce, or barbecue sauce. Other sources are crackers, nuts, bacon, and most processed foods or lunchmeat. Instead, the patient can use fresh onion, garlic, lemon juice, and salt-free or low-sodium salts. Foods high in potassium can affect the heart and muscles. These foods include squash, artichoke, bananas, cantaloupe, oranges, black beans, carrots, and chocolate (Sorrentino & Remmert, 2021).