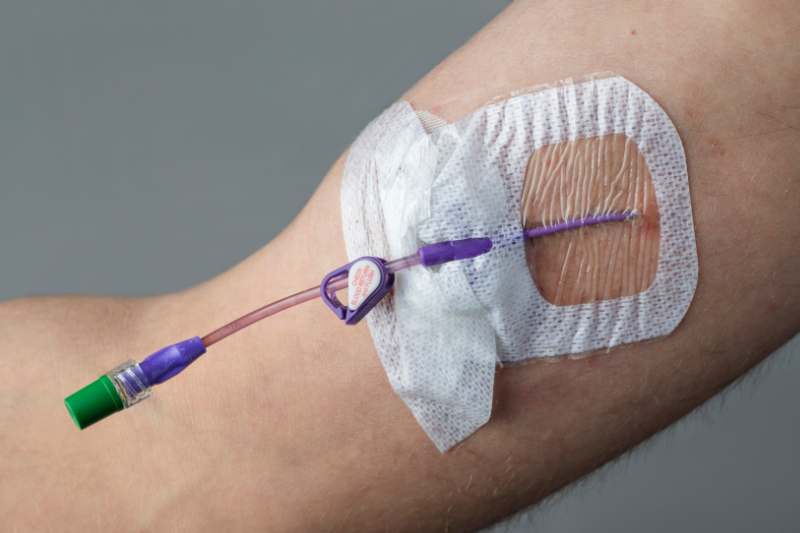
Nursing management of a PICC line includes monitoring for complications and ensuring proper function. First, the insertion site is assessed daily to ensure no signs or symptoms of infection are present. Again, if signs of infection are present, the nurse must contact the healthcare provider, who will most likely order the PICC line removal. Once removed, the tip of the PICC line is sent for culture (CDC, 2025).
Catheter occlusions are one of the most common complications with PICC lines, which can be thrombotic or non-thrombotic. It is imperative for all lumens of the catheter to be flushed at least daily and for the nurse to check medication compatibility if administering two medications through the same lumen. If a catheter becomes occluded, the nurse can first attempt repositioning the patient, as sometimes it's positional. However, the nurse should contact the healthcare provider if the occlusion is still present. The healthcare provider often orders a one-time anticoagulant injection, such as alteplase, through the patient's PICC line to see if this resolves the occlusion (Gonzalez & Cassaro, 2023).
Deep vein thrombosis (DVT) is another potential complication that can develop in the extremity where the PICC line is placed. Signs of a DVT are redness, tenderness, and swelling of the affected extremity. If the nurse suspects a DVT, they should take a measuring tape and measure the circumference of the affected arm. Then, measure the circumference of the unaffected arm and compare it to the affected extremity. If the circumference of the affected extremity is larger, then there is a high suspicion of a DVT. Again, the nurse notifies the healthcare provider immediately if this is suspected, and the provider will most likely order a Doppler ultrasound (Gonzalez & Cassaro, 2023).
Catheter misposition or migration is another common complication of PICC lines; this can occur when the patient strongly coughs during dressing changes or spontaneously. Sometimes, a catheter misposition is found when patients have new cardiac arrhythmias or pneumothorax. If the nurse suspects or knows the catheter has become displaced, they should stop using the PICC line immediately and call the healthcare provider. The provider usually orders an X-ray to confirm its placement (Gonzalez & Cassaro, 2023). Other complications to monitor for include phlebitis, air embolism, and infiltration.