Alzheimer's disease is a progressive neurodegenerative condition that accounts for 60-70% of all diagnosed dementias. Typically, the onset of Alzheimer's disease occurs gradually, often with years of insidious progression before a client or their family brings symptoms of the condition as a concern to a health provider. During these early, quiet years, pathological changes occur in the brain. Extracellular amyloid plaques are being produced and clumping into neurofibrillary (tau) tangles, leading to the loss of crucial neurons and synapses in the brain (Mayeux, 2024).
Table 4: Alzheimer's Blood Test| Good news! New blood tests are about to hit the medical market that can detect the presence of Alzheimer's biomarkers, specifically p-tau217, and give a 90% accurate result on the presence of Alzheimer's. |
| (Hamilton, 2024) |
The diagnosis of Alzheimer's disease is dependent on observable symptoms provoking the use of a verbal or written cognitive assessment test, then confirmation by spinal tap looking for evidence of amyloid plaque components and neurofibrillary (tau) tangles. This is followed by brain imaging such as a positronic emission tomography (PET) scan to see what current brain tissue damage is present. Genetic testing for the gene APOE-e4 (apolipoprotein E) can also be helpful as those having it have been found at higher risk for Alzheimer's Disease and more serious symptoms (Mayo Clinic Staff, 2024a).
Alzheimer's disease is usually observed presenting in these stages (Barker & Gatta, 2024a):
Alzheimer's Stage I: Normal Outward Behavior
This can be years to decades. Silent gradual brain changes begin years before observable symptoms are present.
Alzheimer's Stage II: Very Mild Changes
This lasts around twelve years. There are small indicators, such as forgetting a name or word they often utilize and losing objects such as keys or a shoe. Irritating events that happen to all of us occasionally are increasingly frequent.
Alzheimer's Stage III: Mild Decline
It lasts around seven years. There are more noticeable changes, including having increased difficulty making plans or organizing, forgetting something they just read, trouble remembering the names of those they do not see frequently, and forgetting to pay bills on time.
Alzheimer's Stage IV: Moderate Decline
Lingers around two years. This is when the progressive symptoms begin to be noticed and can include the following:
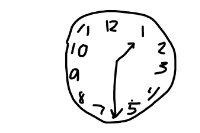
- Difficulty remembering the date.
- Forgetting what month or season it is.
- Trouble cooking or even ordering from a menu.
- Unable to easily use a smartphone.
- Hard to complete multi-step tasks such as cleaning the house.
Alzheimer's Stage V: Moderately Severe Decline
This is around a year to eighteen months in length and is where daily living tasks are affected enough that help is needed. Symptoms can include:
- Trouble remembering where they are and what time it is.
- Difficulty with their own address or phone number.
- Trouble picking out appropriate clothing to wear.
Alzheimer's Stage VI: Severe Decline
This is around two to two and a half years in duration. Symptoms include the following:
- Recognize faces yet not names.
- Mistake people for someone else.
- May need help going to the bathroom.
- Difficulty feeding themselves.
- Weight loss.
- Trouble walking.
- Sleep problems.
Alzheimer's Stage VII: Very Severe Decline
This is the terminal stage of Alzheimer's disease. Many basic abilities, such as walking, eating, swallowing, and sitting up become difficult at this stage. As abilities fade, health assistance grows in importance. Supporting clients and their families is a priority.
Alzheimer's Pneumonia
In Alzheimer's disease, pneumonia is often associated with death. Medical care for both treatment for recovery and symptom control and comfort, up to and including hospice care, becomes the focus for health providers and families.