Several management systems have been developed over the past years in answer to the decreasing availability of health care dollars and the difficulty finding resources for the management of long-term health clients. The advantage of some of the new systems is their ability to be applied to a variety of chronic illnesses, health care settings and target populations, with the end goal of healthier patients, support for health care workers and cost savings throughout the system.
In heart failure, disease management must focus on client and family support following the time of diagnosis with an emphasis on both acute and long-term health supports. In the long term, we must consider the use of community resources to control risk factors, the delivery of supportive medical care, support in life change issues and of course, client tracking. By concentrating on these core components, the client, their family and the health care system all benefit, allowing the client to take on the role of disease management using the support and services of the health care system and community as they control and manage their own life and health.
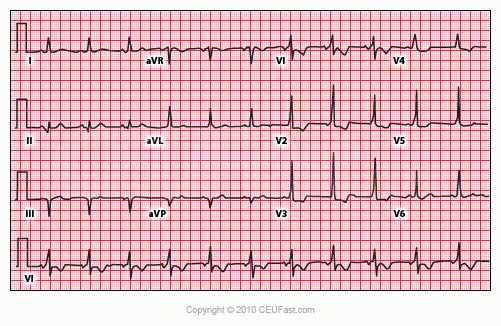
The acute management of a health crisis is often where heart failure is initially recognized and diagnosed. Generally, these are instances of angina, arrhythmias or respiratory difficulties. There are times when the condition is caught earlier in its course by an annual physical as an alert practitioner clues into observable factors. At other times the client or family may make an appointment with a physician to discuss troubling symptoms such as shortness of breath, lack of physical endurance, etc. No matter how it comes about, the time of diagnosis is when chronic management begins.
Once initial stabilization using medication or more invasive procedures is achieved, the physician and treatment team who will be working with the client should meet together with the family and the most important member of the treatment team, the client. Medication, diet, exercise and other lifestyle changes needed to control the symptoms and progression of the condition should at this time be discussed, and a consensus agreement reached. Be aware that not all individuals with a chronic condition such as heart failure will desire to participate in long-term management of their condition. This may be due to the timing, as it may take time for a person to mentally come to the place where they can admit having a life-threatening and life-limiting condition, let alone be prepared to work with it.
Follow-up visits need to be frequently scheduled with treatment team members in order to be able to implement the full range of chronic care management as soon as possible. Until that time, the various members of the treatment team such as physicians, nurses, a social worker, dietician, physical therapist, pharmacist and other specialists (as needed) should work with the family and client to the extent possible. Their mutual goal is to minimize the disease symptoms and increase the client’s participation in their own wellness.
Each area of impact identified in the client's life should be addressed in an individualized, written, treatment plan.
Steps For Negotiating a Treatment Plan:- In clear and simple terms, describe the problem, the management goals, and the potential roles for yourself, your team, and the client in the ensuing care.
- Encourage your client to talk. Prompt them if necessary to state how they see the problem, their goals for treatment, and to raise questions, concerns, fears, or issues.
- Together, discuss questions, concerns, and issues. Reach an agreement on the problem definition and management goals. If you and the client do not agree, be flexible and work to find common ground.
- Remember, it is more important that the client participates and invest themselves in the treatment plan than it is for you to get everything just as you want it to be.
|
Community-based resources can support or expand a health system’s care for chronically ill patients, but traditional health care models are simply not able to make the most of these resources. A single health care provider or institution might form a partnership with a locally based establishment such as a senior center that provides exercise classes in order to leverage an extra advantage to its elderly patients. Yet that is often as far as the effort goes. Buying group memberships for clients in health clubs with individualized trainers, making alliances with massage and physical therapists, seeking hobby level dance groups, walking clubs, cooking clubs, kite flyer groups… the list of possibilities is endless. Ask yourself this…Does your chronically ill client spend afternoons at the zoo rocking the leopard cubs? Do you have former clients visit with the newly diagnosed to explain the life-changing benefits gained from participating in an exercise program? Do you believe that clients only benefit from treatments they hate?
Other organizations and special interest groups can provide information and support to our clients. Departments of health and local public or private agencies often have a wealth of helpful material available for the asking. National organizations such as the American Heart Association or the American Diabetes Association can often help by providing literature, community contacts, and promoting self-help strategies. By looking at the existing resources available all around us, the health care system can enhance care for its patients and avoid duplicating effort.
What it comes down to, is that health care does not just end for the client because they are over an acute episode. A schedule of frequent check-ups combined with weekly status calls from nursing to check on and encourage clients should be a standard practice in chronic management. Many systems that focus on diabetic, coronary artery disease or heart failure patients (for example) have incorporated telephone triage and assessment systems. This allows the client to call in at any time and have an immediate initial response and needs assessment. If a specific health provider needs to call them, that person is informed and can return their phone call in a prompt and practical manner. Routine calls from the treatment nurse assigned to that client can provide support and assessment of ongoing needs. This system has worked well for the management of diabetic clients and clients with histories of cardiac arrhythmias. Health care systems across the country are looking at telephonic systems to provide cost-effective coverage for their clients, keeping them in good condition and away from expensive hospital stays.
Coping successfully with chronic illness means coping with life change. In order to adjust to different lifestyles, diets, activity levels, etc. a person has to be willing and then able to change their life situation. Some measure of support can be gained by community involvement, some from family and friends. As health care professionals we must, first of all, acknowledge that it is the client, and not us, that has the responsibility for that individual’s life decisions. We can offer verbal, technical and resource support, but we cannot make a person change. If they do want to change then frequently scheduled meetings with treatment team members can help to provide them with the information they need to make good decisions. These are also opportune times to offer resources for community and social support, to check on progress and verbally support and encourage. Weekly phone calls can also be encouraging, and no one should have to wait for weeks at a time in order to get an appointment.
So, how is your client doing with their medication changes? Are they having trouble with their new diet? Are they really doing the exercise program you helped them work out as safe to do?
One of the difficulties with the health care system is that we just don’t talk anymore! One visit every three months that is limited by program oversight committees to fifteen minutes or less is simply not adequate. If you cannot call your client and check in on them, maybe a nurse hired just for that purpose can. Telephonic triage systems using trained nurses are becoming an accepted method of maintaining contact and tracking the well-being of clients. Once initial set up costs are made, the long-term gains have been very positive financially. Clients are happy, health care systems can avoid costly emergency room visits, and acute crisis situations can often be avoided, to the relief of insurance companies everywhere!