Once the airway and breathing are stabilized, an initial evaluation of the patient's circulatory status should be performed by palpating central pulses. If a carotid or femoral pulse is verified and no obvious exsanguinating external injury is noted, circulation may momentarily be assumed to be intact. The determination of exact blood pressure should not delay the completion of the primary survey.
While circulation is assessed, two large-bore (16 gauge or larger) IV catheters are placed, most often in the antecubital fossa of each arm, and blood is drawn for testing, particularly for blood typing and crossmatch. Intraosseous cannulation or central venous catheter placement (ideally under ultrasound guidance) can be performed if there is difficulty establishing peripheral IV access.
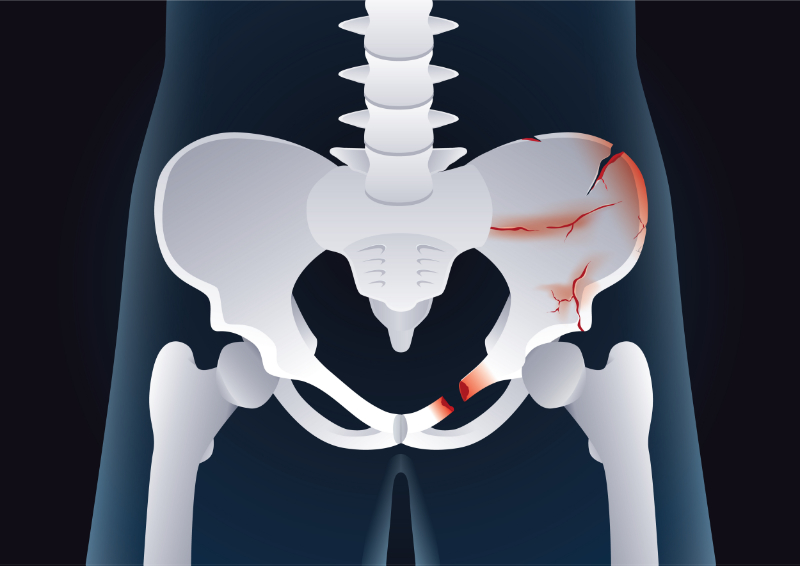
Life-threatening hemorrhage must be controlled. A combination of manual pressure, proximal compression with either a tourniquet or a manual blood pressure cuff, and elevation are typically sufficient to control external arterial hemorrhage. When these are unsuccessful, hemostatic agents may be used, if available. Venous bleeding is controlled with direct pressure. Bleeding from severe pelvic injuries may require the application of a pelvic binder.
Emergency thoracotomy may be needed for trauma patients without femoral or carotid pulses. The procedure is most effective for victims of stab wounds to the chest with pulses or other witnessed signs of life (e.g., voluntary movement). It is rarely beneficial in patients with blunt trauma or when performed in facilities without ready access to appropriate surgical care.
Of note, trauma patients who require cardiopulmonary resuscitation (CPR) within one hour of hospital arrival have a low survival rate to hospital discharge (only 13% in one study), so maintaining perfusion and avoiding the need for CPR is exceptionally important.
In patients in extremis with impending arrest, placement of a resuscitative balloon for occlusion of the aorta (REBOA) by those trained in this technique may be life-saving. This device is most effective in temporizing patients with intra-abdominal or retroperitoneal sources of hemorrhage until more definitive therapy with surgery or angioembolization is possible. So rapid transport to the OR and angiographic suite is essential. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is not appropriate for use in those with suspected thoracic sources of exsanguination or patients in cardiac arrest, in whom emergency department thoracotomy (EDT) should be performed instead.
Most trauma patients with hypotension or signs of shock (e.g., pale, cool, moist skin) are bleeding, and patients with severe hemorrhage have significantly higher mortality.(Table 3)
Table 3 Differential Diagnosis of Shock in TraumaLow CVP* |
- Hypovolemia
- Hemorrhage
- External (compressible)
- Lacerations
- Contusions
- Fractures (partly compressible)
- Internal (noncompressible)
- Intrathoracic
- Intraperitoneal
- Retroperitoneal (partly compressible)
- Fractures (partly compressible)
- Third spacing (e.g., burns)
- Neurogenic (high cervical cord injury)
|
High CVP* |
- Pericardial tamponade
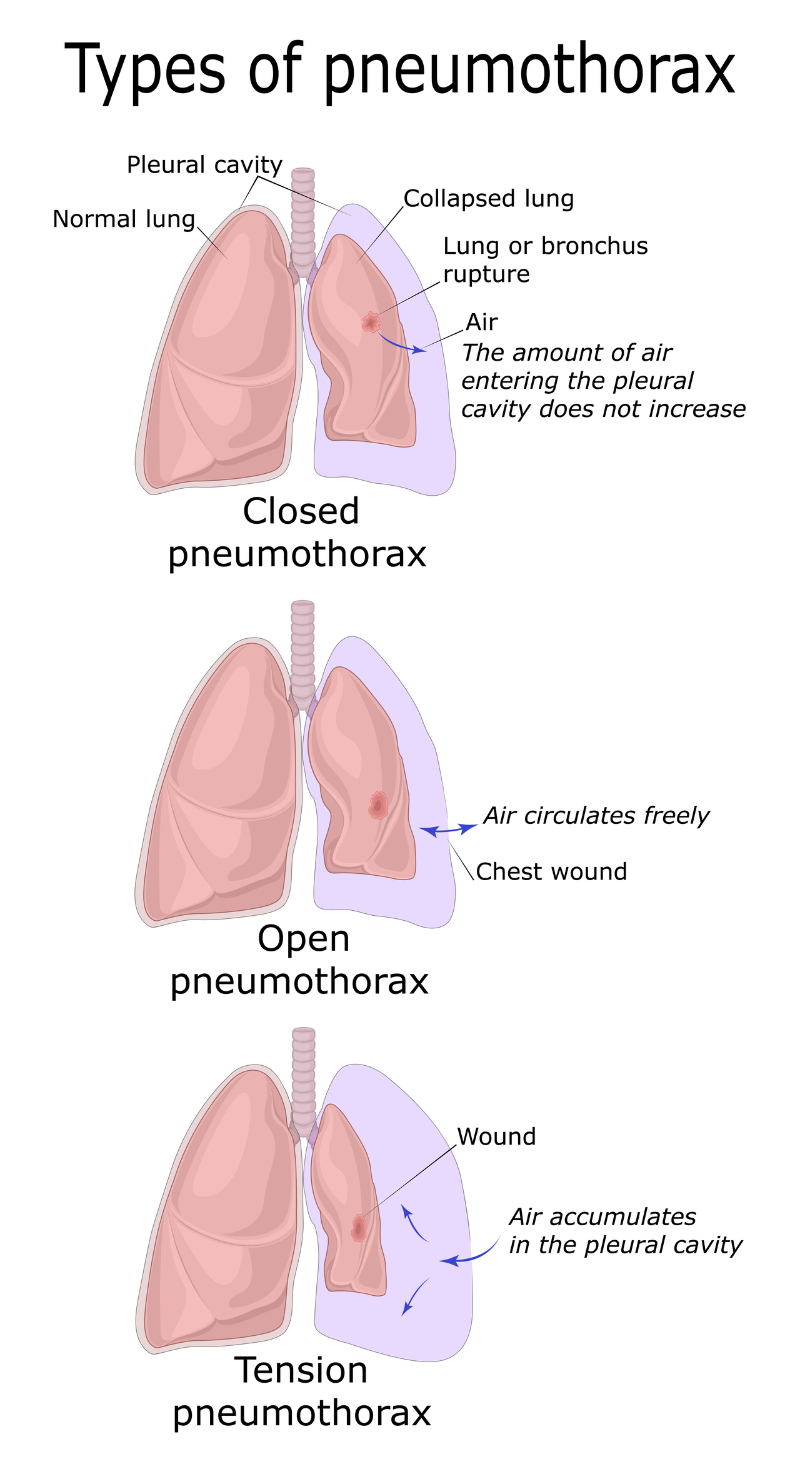
- Tension pneumothorax
- Myocardial contusion
|
Other Diagnoses to Consider |
- Pharmacologic or toxicologic agents
- Myocardial infarction (MI) (severe)
- Diaphragmatic rupture with herniation
- Fat or air embolism
|
*CVP: central venous pressure
Initial fluid resuscitation for these patients may consist of a bolus of IV crystalloid (e.g., 20 mL/kg isotonic saline). However, patients with obvious severe or ongoing blood loss should be transfused immediately with type O blood (women of childbearing age should be transfused with O negative blood). While mildly unstable patients may be treated with isotonic crystalloid instead of blood, the unnecessary crystalloid infusion should be avoided.
Despite an initial fluid bolus, patients with persistent hemodynamic instability generally require blood transfusion and definitive control of the bleeding source. Significant hemorrhage occurs in any of five sites:
- External
- Intraperitoneal
- Intrathoracic
- Long bone fractures
- Pelvic fractures
- Retroperitoneal
A 1:1:1 ratio of plasma, platelets, and red cells should be targeted if transfusion is required. Patients requiring transfusion may benefit from treatment with tranexamic acid (an antifibrinolytic agent) if given within three hours of injury.
It is important to obtain manual blood pressure measurements in trauma patients with systolic blood pressures below 90 mmHg, as automated blood pressure cuffs often overestimate values significantly in these patients. Furthermore, data suggest that the traditional threshold of a systolic blood pressure below 90 mmHg to define shock is inaccurate. The appropriate systolic or mean arterial blood pressure threshold for defining shock varies by age. A significant proportion of trauma patients with hemorrhagic shock have systolic blood pressure above 90 mmHg. Using a cut-off of 110 mmHg is likely to be more appropriate in the elderly.