GERD: Navigating Gastroesophageal Reflux
Written by Mariya Rizwan, PharmD
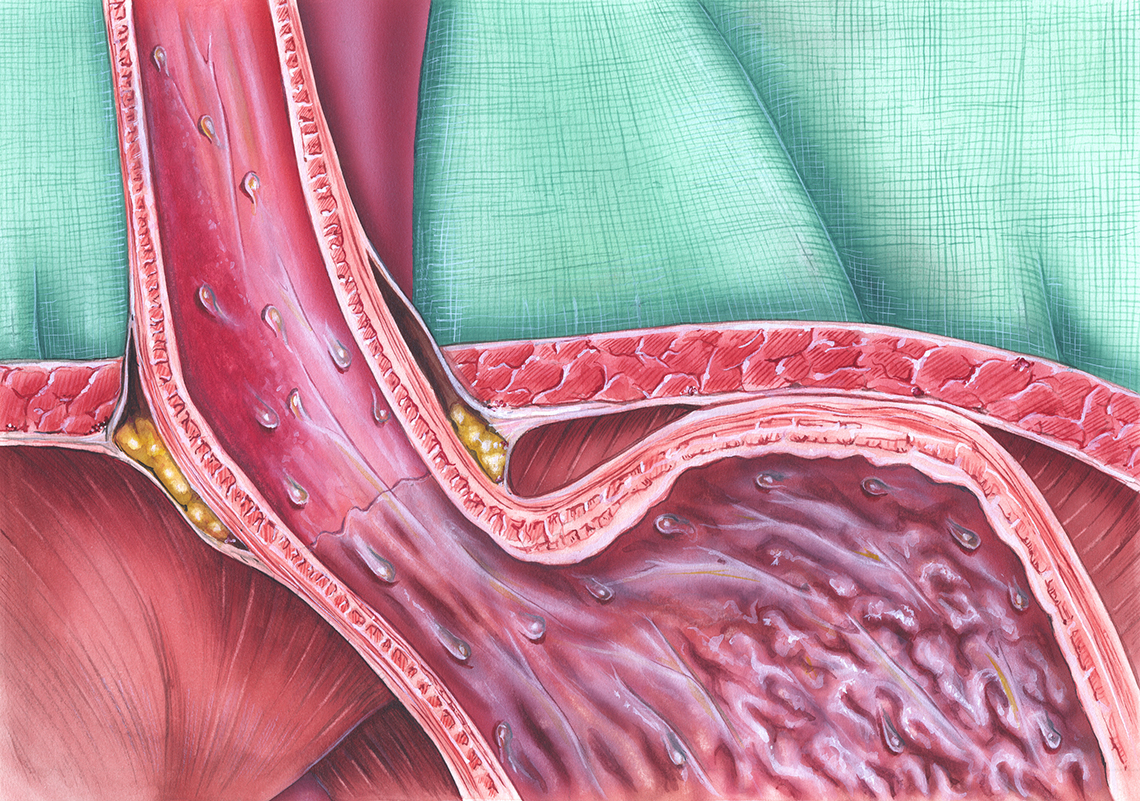
GERD, also known as gastroesophageal reflux disease, is a prevalent condition affecting approximately 40% of individuals at some point during their lifetime. This syndrome arises due to the retrograde movement of stomach contents back into the esophagus, a phenomenon often referred to as esophageal reflux. The primary cause of GERD is the improper relaxation of the lower esophageal sphincter (LES), which usually acts as a barrier to prevent gastric contents from entering the esophagus. This relaxation occurs in response to an unidentified stimulus. While GERD is predominantly observed in adults, it is essential to note that this condition can also affect children, albeit less frequently.
If the reflux occurs regularly, the esophagus can’t tolerate it, damaging its mucosa. It can lead to tissue injury, inflammation, hyperemia, and even erosion without protection. In healing, the replaced normal squamous cell epithelium may be more resistant to reflux but may also be a premalignant tissue that can lead to adenocarcinoma. Long-term exposure to acid may also lead to fibrosis and scarring, which can cause esophageal stricture, leading to difficulty in swallowing. Chronic reflux is often associated with hiatal hernia.
What Causes GERD?
There are no exact reasons for GERD. Some people are sensitive to triggers such as:
- Peppermint
- Coffee
- Fatty and fried food intake
- Alcohol
- Chocolates
- Nicotine consumption
Drugs that can cause GERD include non-steroidal anti-inflammatory drugs (NSAIDs), beta-adrenergic blockers, nitrates, certain antibiotics, theophylline, and anticholinergic drugs.
Aging, obesity, and physical inactivity may also play a role in increased acid reflux.
Symptoms of GERD
- Dyspepsia or pyrosis
- Difficulty swallowing or dysphagia
- Painful swallowing or odynophagia during eating
- Eructation, flatulence, or bloating after eating
- A substernal or retrosternal pain that radiates upward to the neck, jaw, or back; the pain worsens when a patient bends over, strains, or lies flat.
If severe inflammation is present, discomfort occurs after each meal and remains for up to two hours.
The patient may also complain about cough, hoarseness, or wheezing at night, accompanied by regurgitation and the sensation of warm fluid traveling upward to the throat and leaving a bitter, sour taste in the mouth.
Sometimes, the patient may also experience weight loss due to poor dietary intake.
Implementation
Generally, dietary restrictions can help manage GERD symptoms. But sometimes, pharmacological treatment is also given, such as:
- Antacids like aluminum or magnesium salts relieve heartburn by neutralizing gastric acid.
- Proton pump inhibitors such as omeprazole, esomeprazole, rabeprazole, lansoprazole, and dexlansoprazole are the most potent agents against GERD; they work by blocking the parietal cells' final step in the H+ ion secretion.
- H2 receptor antagonists include cimetidine, ranitidine, famotidine, and nizatidine; they act as competitive antagonists against histamine and bind reversibly to the H2 receptors in the gastric parietal cells, inhibiting histamine's activity.
- Dopamine receptor antagonists, such as metoclopramide, work as a gastrointestinal stimulant by improving gastric emptying and increasing pressure on the lower esophageal sphincter.
- Sucralfate is a supportive treatment that forms a protective adhesive gel over areas of injury or inflammation.
Nurses should guide the patient in making dietary restrictions. Educate them to avoid consuming fatty foods, caffeinated beverages, chocolate, nicotine, alcohol, and peppermint. Patients should not consume spicy food during acute inflammation as it can interfere with healing.
Encourage the patient to consume five to six small meals daily instead of two large meals, as consuming too much at a time can increase gastric pressure and lead to increased gastroesophageal reflux.
Weight loss and smoking cessation programs are also essential for patients who are obese or smoke cigarettes. Also, inform the patient that lying straight can increase acid reflux. Therefore, elevating the head of the bed during sleep may mitigate symptoms. Place 6-inch blocks under the head of the bed or place a wedge under the mattress to enhance nocturnal acid clearance. The patient should also avoid eating food at least three hours before bed.
Lifestyle modifications also help the management of GERD. If the patient is overweight or obese, compel them to lose weight as fat causes increased intra-abdominal pressure. Encourage the patient to avoid restrictive clothing, lifting heavy objects, straining, working in a bent-over position, and stooping. Educate the patient to avoid consuming alcohol, chocolate, coffee, citrus fruit, and tomatoes. Refer them to a dietician who can help them shed extra pounds and guide them about appropriate dietary intake.
The Bottom Line
GERD can be managed well with dietary restrictions, lifestyle modification, and pharmacological treatment. As a nurse, guide the patient about making appropriate lifestyle modifications.
Patients who do not respond well to pharmacological treatment might need surgical intervention such as Nissen fundoplication, Hill repair, and Belsey repair. Ask your patients to attend follow-up visits and report to you any adverse drug reactions or worsening symptoms.
About the Author:
Mariya Rizwan is an experienced pharmacist who has been working as a medical writer for four years. Her passion lies in crafting articles on topics ranging from Pharmacology, General Medicine, Pathology to Pharmacognosy.
Mariya is an independent contributor to CEUfast’s Nursing Blog Program.
Please note that the views, thoughts, and opinions expressed in this blog post are solely of the independent contributor and do not necessarily represent those of CEUfast. This blog post is not medical advice. Always consult with your personal healthcare provider for any health-related questions or concerns.
If you want to learn more about CEUfast’s Nursing Blog Program or would like to submit a blog post for consideration, please visit https://ceufast.com/blog/submissions.