Barbiturates are CNS depressant drugs used for their sedative and hypnotic effects. They include:
- amobarbital
- butalbital
- methohexital
- pentobarbital
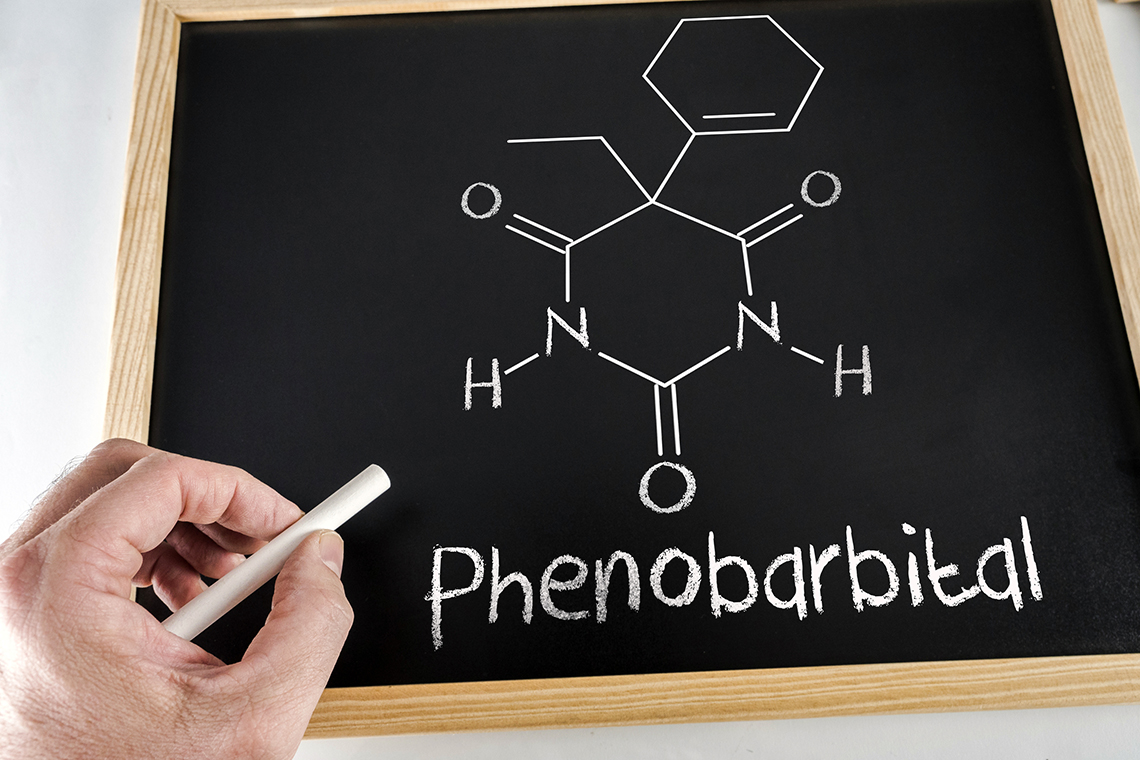
- phenobarbital
- primidone
They are well absorbed from the gastrointestinal tract, rapidly distributed in the body, metabolized by the liver, and excreted in urine.
Barbiturates exert their sedative and hypnotic effects by depressing the sensory cortex of the brain, decreasing its motor activity, and altering cerebral function, hence producing drowsiness, sedation, and hypnosis. They act throughout the CNS, but the reticular activating system (RAS) of the brain, which is responsible for wakefulness, is a particularly sensitive site.
Barbiturates have various clinical indications other than sedative and hypnotic actions. They are used:
- To sedate the patient in the daytime- for short periods, often less than two weeks
- To provide relief from insomnia
- For anesthesia and preoperative sedation
- To provide relief from anxiety
- In seizures for their anticonvulsant effects
Actions
Barbiturates work by:
- Inducing an imbalance between central inhibitory and facilitatory mechanisms, which influences the cerebral cortex and reticular formation
- Decreasing the presynaptic and postsynaptic membrane excitability
- Producing depression at all levels of the CNS that can lead to mild sedation to coma and eventually death
- Facilitating the action of inhibitory neurotransmitters in the brain known as GABA
- Exerting a central effect in the brain that causes respiratory depression and slows gastric motility
- Reducing nerve transmission and decreasing the excitability of the nerve cells- the principal anticonvulsant mechanism of action of barbiturates
- Raising the seizure threshold
Compared to benzodiazepines, tolerance can occur to barbiturates even in small doses and rapidly. In comparison, benzodiazepines are quite safer and relatively more effective than barbiturates. For these reasons, they have replaced barbiturates as the choice of sedatives and hypnotics.
Contraindications and Precautions
Barbiturate use is contraindicated in patients with known hypersensitivity to it, comatose patients, or those with preexisting CNS depression, known alcohol intolerance, severe pre-existing pain, and severe respiratory disease with obstruction and dyspnea.
It should not be given to lactating mothers. Either their drug intake should be stopped, or the baby should be shifted to bottle feed. Chronic use of barbiturates during pregnancy can result in drug dependency in the infant and may also result in fetal malformation and coagulation defects in the fetus. Acute use at full term may lead to respiratory depression in the newborn.
Barbiturates should be used cautiously in patients with hepatic dysfunction and a history of suicide attempts or drug abuse. For hypnotic use, they should be given for a very short time as chronic use leads to dependence.
Barbiturates should be given in the initial dose for the elderly population, and the dose should be titrated accordingly.
Drug Interactions
Various drug interactions can occur with barbiturates. They may reduce the effects of beta-blockers, such as propranolol, bisoprolol, and metoprolol. Moreover, they decrease the effects of corticosteroids, oral anticoagulants, chloramphenicol, hormonal contraceptives, tricyclic antidepressants, quinidine, metronidazole, cyclosporine, and theophylline.
When given with phenobarbital, hypantoines such as phenytoin can reduce its metabolism, leading to increased toxic effects of phenobarbital. In these cases, dose adjustment is necessary.
Methoxyflurane, when given with barbiturates, produces nephrotoxic metabolites. Therefore, their concomitant use should be avoided, especially in renal-compromised patients. Moreover, barbiturates with other CNS depressants can potentiate CNS depression. Therefore, avoid administering any other CNS depressant with barbiturates.
Valproic acid may increase serum barbiturate levels, eventually causing increased effects, such as sedation, hypnosis, and even respiratory depression.
Monoamine oxidase inhibitors, such as phenelzine, selegiline, and tranylcypromine, slow the barbiturate metabolism, increasing sedative and hypnotic effects. When barbiturates are given with acetaminophen, the risk of liver toxicity is increased.
Side Effects
Barbiturates cause side effects, such as lethargy, drowsiness, headache, depression, hypotension, and bradycardia. Respiratory side effects of barbiturates include hypoventilation, reduced breathing rate, spasms of the larynx and bronchi, and severe respiratory depression. Other general side effects include nausea, vomiting, vertigo, and epigastric pain.
Nursing Considerations
Before starting barbiturate therapy, assess the patients condition, level of consciousness, and sleeping pattern. These parameters should also be monitored with ongoing therapy. This helps determine whether the drug is effective. Furthermore, check the patients neurologic status for alteration or deterioration with barbiturate therapy.
When administering barbiturates parenterally, avoid extravasation, which can lead to local tissue damage and necrosis. Administer the drug via an intravenous (IV) route or deep intramuscular (IM) injection, but do not exceed 5 milliliters (ml) for IM administration.
Too rapid IV administration of barbiturates can cause respiratory depression, apnea, laryngospasm, and hypotension. If it happens accidentally, be prepared to resuscitate the patient. Also, keep an eye on the patient for seizures with barbiturate therapy. Check the character, frequency, and duration of seizures and note any changes in seizures if they occur.
Practice safety measures to prevent falls and injuries. Educate the patient to stand slowly from lying and sitting positions. When sleeping, raise their side rails, keep the call light within reach, and assist them in getting out of bed. Ask the patient to keep their most useful things on their side tables so they can easily access them from the proximity of their bed.
Monitor the serum drug levels of barbiturates closely. Their therapeutic levels range from 15 to 40 micrograms (mcg)/ml. If more than that, contact the healthcare provider. Observe the patient closely and prevent hoarding and self-dosing. Educate them to take the drug only in the prescribed doses. If they cant sleep well with the dose, ask them to inform you. Keep a keen eye on the patient if they are getting depressed, are suicidal, or have become drug dependent with barbiturate therapy. If you notice any of these signs, inform the healthcare provider promptly.
To stop the drug, taper it off slowly, as stopping it altogether can cause severe withdrawal symptoms, and seizures can worsen.
With long-term barbiturate therapy, patients lab tests should be monitored closely, as they can alter them. Monitor renal and hepatic functions. Also, serum folate concentration should be monitored periodically because patients with seizure disorders have increased folate requirements with long-term barbiturate therapy. They may also cause decreased serum bilirubin concentrations in neonates, especially in patients with congenital nonhemolytic unconjugated hyperbilirubinemia and in people with epilepsy. When given in higher than normal doses, barbituates can lead to toxicity. The symptoms of barbiturate toxicity include confusion, drowsiness, slurred speech, staggering, and dyspnea. If you notice any of these signs in your patients reviving barbiturate therapy, report to the healthcare provider promptly.
Patient Teaching
With barbiturate therapy, it is essential to educate the patient and their caregivers. Educate them that barbiturates can cause physical and psychological dependence. If they feel they cant survive without the medication and need it for their survival, inform the healthcare provider promptly. Moreover, educate them to take the drug as prescribed, not to change the dose on their own or combine any other drug with it, especially CNS depressants. They should not combine any over-the-counter medicines or herbal remedies with barbiturate therapy without consulting their healthcare provider.
Educate them that morning hangovers can occur after the therapeutic use of barbiturates. Visit the healthcare provider if they find the symptoms too bothersome. Moreover, they should avoid doing hazardous tasks, driving a motor vehicle, or operating machinery while on barbiturate therapy. Also, they should review other safety measures with the healthcare provider to prevent falls and injury.
Encourage them to inform the healthcare provider if they have a complaint of vertigo with the therapy. Furthermore, barbiturates take 2-3 weeks to show their full effects, except when a loading dose is used. Educate them not to stop the barbiturate intake abruptly. It has to be stopped bit by bit so abrupt withdrawal symptoms do not occur. Also, educate them not to drink alcohol with ongoing therapy as both can depress the CNS, leading to life-threatening consequences.
Inform them that barbiturates interact with contraceptives. Therefore, they should use something else for contraception, such as condoms, to avoid getting pregnant unplanned. Ask them to report to you if they have any skin eruptions or significant side effects with ongoing barbiturate therapy.
Advise the patient to notify the healthcare professional promptly if they have signs and symptoms of angioedema, sore throat, fever, mouth sores, bruising, or unusual bleeding with barbiturate therapy.
Teach patients about sleep hygiene techniques, such as maintaining a dark room while sleeping, having a quiet and peaceful environment with optimal temperature to sleep, avoiding daytime napping, and avoiding too much nicotine or caffeine intake throughout the day, especially at night.
For the pediatric population, advise the parents and caregivers that barbiturates may cause irritability, hyperactivity, and sleep disturbances in the child that may take some time, from a few days to a few weeks, to diminish, or it may persist until the drug is stopped. In severe cases, an alternative medication can be considered. Parents or caregivers should report to the healthcare professional if the child is extremely irritable with barbiturate therapy. Instruct the parents to monitor the childs skin closely for any rash occurring 7 to 20 days after the treatment begins.
Teach the family about symptoms of barbiturate toxicity that include drowsiness, staggering, and slurred speech. Tell them to promptly bring the patient to the hospital if they notice these symptoms.
The Bottom Line
Barbiturates are used for deep sedation and hypnosis purposes. However, they should be given in the least possible doses because of their potent CNS depressant activities. If given in high doses, it can cause respiratory depression.
Compel your patients to attend follow-up visits if they take barbiturates, report to the healthcare provider if they have any adverse effects, and do not stop the drug intake abruptly, especially when given for seizure control.
About the Author:
Mariya Rizwan is an experienced pharmacist who has been working as a medical writer for four years. Her passion lies in crafting articles on topics ranging from Pharmacology, General Medicine, Pathology to Pharmacognosy.
Mariya is an independent contributor to CEUfast's Nursing Blog Program. Please note that the views, thoughts, and opinions expressed in this blog post are solely of the independent contributor and do not necessarily represent those of CEUfast. This blog post is not medical advice. Always consult with your personal healthcare provider for any health-related questions or concerns.
If you want to learn more about CEUfasts Nursing Blog Program or would like to submit a blog post for consideration, please visit https://ceufast.com/blog/submissions.