Chronic disease poses a significant challenge to the healthcare system globally. Conditions such as diabetes, heart failure, chronic obstructive pulmonary disease (COPD), and many others often require ongoing management, frequent monitoring, and adherence to complex treatment plans. Patients may struggle with medication adherence, experience frequent hospitalizations, and face limited access to quality care, particularly in rural or underserved areas.
Remote Patient Monitoring (RPM) offers a solution to address these challenges and improve the quality of care for individuals living with chronic conditions. By using technology to monitor patient health status from a distance, RPM empowers patients to actively participate in their own care, enhances communication between patients and healthcare providers, and improves healthcare delivery's overall efficiency and effectiveness.
What is Remote Patient Monitoring?
Remote Patient Monitoring (RPM) involves continuously monitoring a patient's health status outside a traditional healthcare setting using various technological tools. This may include:
- Telehealth platforms to help facilitate virtual consultations between patients and healthcare providers, enabling remote assessment, diagnosis, and treatment adjustments.
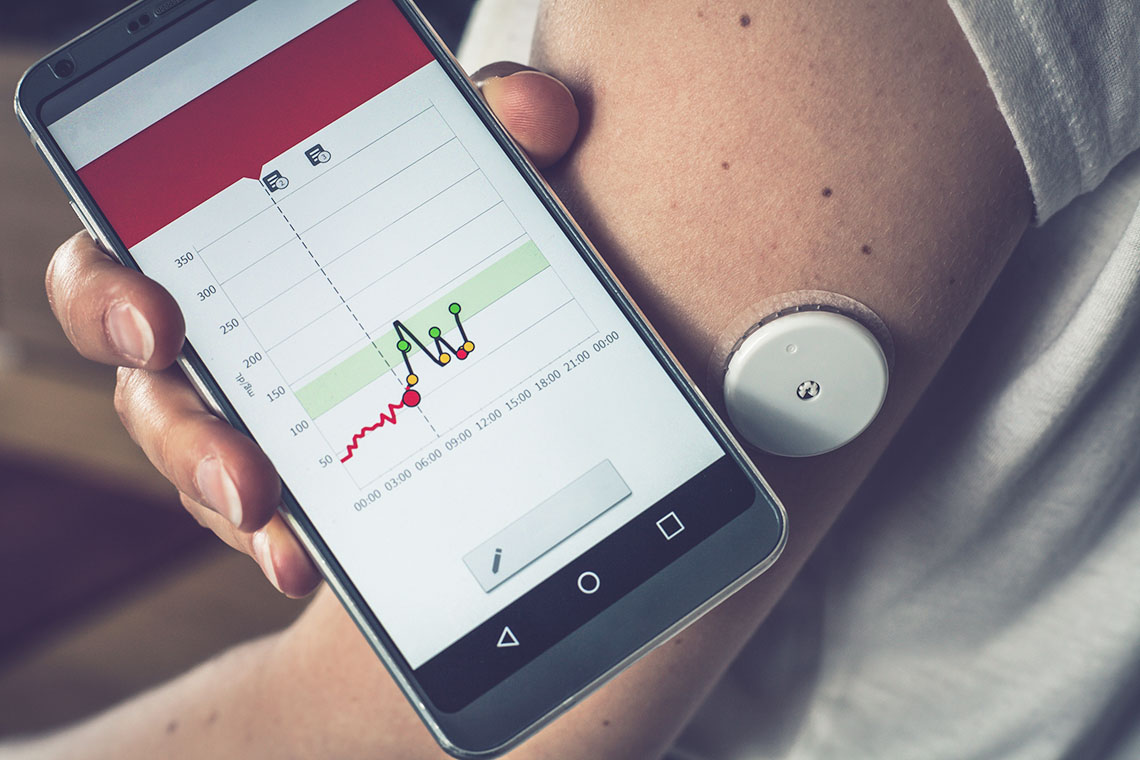
- Wearable devices, such as smartwatches, blood pressure monitors, glucose meters, and activity trackers, collect real-time data on vital signs, activity levels, and other health metrics.
- RPM, such as software platforms and mobile applications, enable the secure transmission and storage of patient data, allowing healthcare providers to access and analyze information remotely.
Benefits of RPM for Chronic Disease Management
RPM offers numerous benefits for both patients and healthcare providers in managing chronic diseases. It allows people with chronic diseases to track their data and make real-time decisions for their treatments.
Improved Patient Outcomes
Allowing remote monitoring can improve patient treatment outcomes. Several devices can help patients manage treatment in their daily lives. RPM can be used in hospitals and other settings outside the home.
RPM can significantly improve medication adherence rates by providing real-time feedback on medication adherence and identifying potential issues early. Proactive monitoring of vital signs and early detection of complications can help prevent acute exacerbations and reduce the risk of hospital readmissions.
RPM can enhance patients' overall quality of life by empowering them to actively manage their condition and giving them greater control over their health. Continuous monitoring allows for the early detection of potential complications, enabling timely interventions and preventing disease progression.
Enhanced Patient Engagement
RPM provides patients with valuable insights into their health, empowering them to make informed decisions about their care and actively manage their condition. This increases patient empowerment and self-management of conditions.
Another benefit is that RPM can improve communication and collaboration between patients and healthcare providers. It facilitates seamless communication and collaboration, enabling more frequent and personalized interactions.
Communication software allows patients to interact with their doctor's office, view current results, and contact the office directly with any questions.
Improved Efficiency and Cost-Effectiveness
RPM can significantly reduce healthcare costs by preventing complications and reducing the need for hospitalizations and emergency visits. It allows healthcare providers to allocate their time and resources more efficiently by focusing on patients who require the most immediate attention.
This can be seen with telemetry readings and other monitors, which can be used both at home and in a healthcare facility.
The Role of Nurses in RPM
Nurses play a crucial role in successfully implementing and managing RPM programs. As technology advances, nurses will need to stay up to date with current healthcare devices.
- Data Interpretation and Analysis:
- Continuously monitoring patient data for trends and anomalies.
- Identifying potential health risks and escalating concerns to the appropriate healthcare providers.
- Patient Education and Support:
- Providing comprehensive education to patients on the use of RPM devices and the interpretation of data.
- Guiding patients on lifestyle modifications and self-management techniques like diet, exercise, and stress management.
- Offering emotional support and addressing patient concerns related to their condition and the use of RPM technology.
- Telehealth Consultations:
- Participating in virtual consultations with patients and other healthcare providers.
- Assessing patient needs and adjusting care plans based on real-time data and interactions.
RPM for Specific Chronic Conditions
RPM has shown significant promise in managing a wide range of chronic conditions.
Diabetes:Continuous Glucose Monitoring (CGM) systems provide real-time data on blood sugar levels, allowing for more precise insulin dosing and better control of blood sugar fluctuations. Insulin pumps can be remotely adjusted by healthcare providers based on real-time CGM data, optimizing insulin delivery.
Remote blood sugar monitoring enables patients to easily transmit their blood sugar readings to their healthcare providers, facilitating timely interventions.
Heart Failure:Remote blood pressure and heart rate monitoring allows for early detection of worsening heart failure symptoms, such as fluid overload or worsening arrhythmias.
Weight monitoring helps track fluid retention and assess the effectiveness of diuretic medications. Fluid intake tracking can assist patients in adhering to fluid restrictions.
Chronic Obstructive Pulmonary Disease (COPD):Peak flow meters can be used to monitor lung function and identify early signs of an exacerbation. Pulse oximeters can continuously monitor blood oxygen saturation levels, alerting patients and healthcare providers to potential respiratory distress.
Challenges and Considerations
While RPM offers significant potential, several challenges and considerations must be addressed for its successful implementation:
- Data privacy and security concerns
- Technological limitations and disparities
- Reimbursement challenges
- Ensuring patient data accuracy and reliability
- The need for adequate training and support for healthcare providers
RPM has the potential to revolutionize the management of chronic diseases by empowering patients, improving communication between patients and healthcare providers, and enhancing the efficiency and effectiveness of healthcare delivery. By addressing the challenges and considerations outlined above, we can unlock RPM's full potential to improve the lives of millions of people living with chronic conditions.
Continued research and innovation in RPM are crucial to refining existing technologies, developing new and innovative solutions, and ensuring equitable access to these transformative technologies for all. The future of RPM holds immense promise for transforming healthcare delivery and improving patient outcomes globally.
About the Author:
Breann Kakacek, BSN, RN, has been a registered nurse since 2015 and a CNA prior to that for two years while going through the nursing program. Most of her nursing years included working in the medical ICU, cardiovascular ICU, and the OR as a circulating nurse. She has always had a passion for writing and enjoys using her nursing knowledge to create unique online content. You can learn more about her writing career and services at ghostnursewriter.com
Breann is an independent contributor to CEUfast's Nursing Blog Program. Please note that the views, thoughts, and opinions expressed in this blog post are solely of the independent contributor and do not necessarily represent those of CEUfast. This blog post is not medical advice. Always consult with your personal healthcare provider for any health-related questions or concerns.
If you want to learn more about CEUfasts Nursing Blog Program or would like to submit a blog post for consideration, please visit https://ceufast.com/blog/submissions.