Understanding the Mpox Outbreak: Key Facts for Healthcare Workers
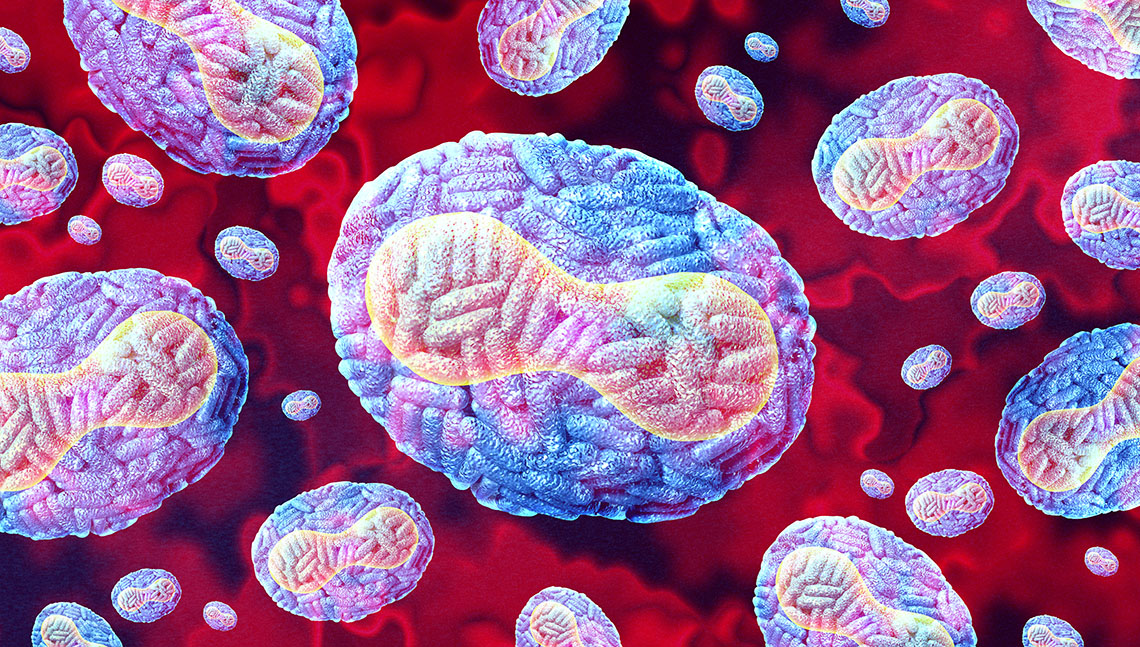
The recent increase in Mpox (Monkeypox) cases has captured the global healthcare community's attention. Once thought to be a rare zoonotic disease, the current outbreak has quickly spread across continents, prompting the World Health Organization (WHO) to declare it a public health emergency. This pandemic has raised concerns about public health readiness and the possibility of widespread transmission as it has unexpectedly spread beyond its usual regions in Africa to countries all over the world, including the United States.
As the virus started to spread, it became evident that this was not a typical outbreak. Unlike previous instances where the virus stayed localized, this outbreak showed a worrying ability for sustained human-to-human transmission in various ways, including respiratory droplets, skin contact, and sexual transmission. This new understanding of the virus's spread led global health authorities to issue warnings and advisories, causing widespread public concern.
Mpox Through the Decades
Mpox was first identified in humans in 1970 in the Democratic Republic of Congo. Initially, it was primarily confined to Central and West African countries, where it is endemic. The virus belongs to the Orthopoxvirus genus, which also includes the now-eradicated smallpox virus. Mpox outbreaks have occurred sporadically in Africa over the decades, but they were generally contained and did not lead to widespread outbreaks.
Previous outbreaks outside Africa, such as the 2003 outbreak in the United States linked to imported animals, were limited in scope and did not spread extensively. However, the current situation is unprecedented as it marks the first time that mpox has spread so widely and rapidly on a global scale. This has prompted comparisons to other global health emergencies, although the public health implications of mpox are distinct from those of previous pandemics.
Unlike past outbreaks, which were mainly limited to zoonotic transmission, the current outbreak is characterized by sustained human-to-human transmission, particularly in social and sexual networks. As a result, public health strategies have shifted to focus on identifying and isolating cases, educating the public about transmission risks, and ensuring access to vaccines and treatments.
What Healthcare Professionals Need to Know about Mpox
Healthcare professionals are crucial frontline responders in controlling the spread of mpox. Their understanding of the virus's transmission, symptoms, and available treatments is essential in managing and mitigating the outbreak. As this outbreak has a global reach, it is more important than ever for healthcare workers to be well-versed in the latest guidelines and recommendations.
The disease typically presents with flu-like symptoms and a characteristic rash, similar to smallpox but generally less severe.
There are two known types, or clades, of the mpox virus:
- Clade I (Central African clade): This type is more severe and historically has been responsible for higher mortality rates in the regions where it is endemic.
- Clade II (West African clade): This type is generally associated with milder disease and lower mortality rates.
The current global outbreak, which began in 2022 and continues into the present, is caused by clade IIb, a subtype of the West African clade. While less severe than the Central African clade, this particular strain has demonstrated a capacity for widespread human-to-human transmission, which is unusual for mpox.
Why Is Clade IIb Significant?
Clade IIbs ability to spread rapidly, even outside its typical endemic regions, has made it a public health concern. Although the symptoms caused by this clade are generally milder than the Central African clade, the virus's transmissibility and the ease with which it has crossed international borders have led to its designation as a global pandemic.
Healthcare professionals should be particularly aware of the transmission dynamics of clade IIb, especially in non-endemic regions where public awareness may be lower. Understanding the specifics of this clade helps identify and manage cases effectively, ensuring appropriate measures are taken to prevent further spread.
Transmission:
Mpox primarily spreads through close contact with an infected person or animal or by contact with contaminated materials such as bedding or clothing. It can also be transmitted from human to human through respiratory droplets, direct contact with skin lesions, or bodily fluids. The virus can even spread through sexual contact, so healthcare providers must understand its various modes of transmission in different populations.
Symptoms:
Incubation Period:
- Typically 7 to 14 days, but can range from 5 to 21 days
Initial Symptoms:
- Fever
- Headache
- Muscle aches
- Fatigue
Rash Development:
- Starts on the face and spreads to other parts of the body
- Progresses through several stages: macules, papules, vesicles, pustules, and then scabs
Lymphadenopathy:
- Swollen lymph nodes are a common symptom that helps differentiate mpox from other poxvirus infections
Treatments:
At the moment, no specific antiviral treatment has been approved for mpox. However, healthcare professionals can help manage symptoms and prevent complications through supportive care. This includes managing pain, preventing secondary infections, and addressing any other complications that may arise. In severe cases, antiviral medications such as tecovirimat (TPOXX) may be considered under compassionate use protocols, as they have shown some effectiveness against Orthopoxviruses in investigational laboratory settings.
Vaccines:
The smallpox vaccine effectively prevents mpox infection because of the genetic similarities between the two viruses. In response to the current outbreak, vaccination campaigns using modified vaccinia Ankara (MVA) and ACAM2000 vaccines are being deployed in affected regions. Healthcare providers should be aware of the availability of these vaccines and the protocols for administering them, especially to high-risk populations.
As healthcare professionals, it is essential to stay updated on the latest developments in the mpox pandemic. This includes knowing new case definitions, treatment protocols, and vaccination strategies. Continued education and training ensure healthcare workers can effectively identify and manage mpox cases.
What Else Do We Need to Know?
Although the global spread of mpox is concerning, it is essential to approach the situation with a balanced perspective. The virus is more transmissible than initially thought, but it is less contagious than many other infectious diseases, such as COVID-19. The availability of effective vaccines and the relatively lower mortality rate of mpox compared to other Orthopoxviruses are reassuring factors.
Healthcare professionals must remain vigilant, informed, and prepared to manage cases as they arise. Ongoing monitoring of the situation, along with public health interventions such as vaccination and education, will be critical in controlling the spread of the virus.
In summary, while mpox poses a significant public health challenge, the tools and knowledge required to manage the outbreak are within reach. By staying informed and prepared, healthcare professionals can play a crucial role in protecting public health and mitigating the impact of this pandemic.
**In response to the escalating global mpox cases, CEUfast, a leading provider of continuing education for healthcare professionals, has made its Mpox Course free. This initiative aims to ensure that nurses and other healthcare workers have immediate access to the critical knowledge required to manage and mitigate the outbreak's impact.