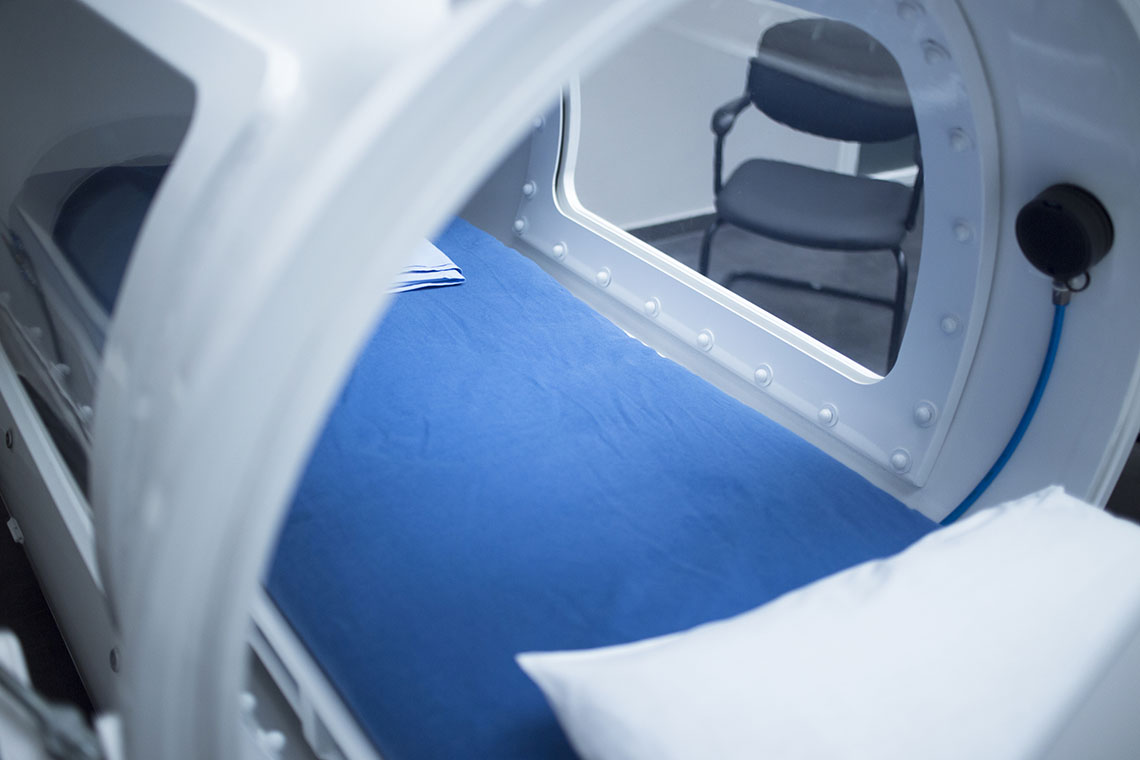
The uniqueness of the nursing profession is evident in the diverse opportunities to work in different settings. I remember when I worked as a registered nurse in a medical intensive care unit (MICU), I had to transport my patient to the hyperbaric oxygen therapy department. As a fairly new critical care nurse, I remember being anxious when transporting my patient anywhere outside of the unit. It could have been to a computerized tomography (CT) scan, a magnetic resonance imaging (MRI), or to interventional radiology. It did not matter. It felt like a layer of my safety net was lost once I left the MICU. When we arrived at the hyperbaric oxygen therapy department, the nurse made us feel very comfortable. She was very knowledgeable and allowed me to walk through the chamber before the patient went into it. I still have a picture of my patient care technician posing in front of the chamber. I was fascinated with this huge piece of equipment that looked like a submarine.
Prior to actually seeing this for myself and the mention of it in nursing school, the most prominent memory of a hyperbaric chamber was when I was much younger. There were rumors in the tabloids that celebrities would sleep in hyperbaric chambers to live forever. Of course, now I know that a hyperbaric oxygen chamber is not the key to immortality; however, it is certainly an innovative key to healing. After that experience with transporting my patient, I actually contemplated transitioning to the role of hyperbaric nurse. I just was not sure what that transition would look like.
So, what do you think about hyperbaric nursing? Never heard of it? Sounds interesting? Keep reading!
What is Hyperbaric Oxygen Therapy?
Hyperbaric oxygen therapy is a treatment where patients breathe pure oxygen in a pressurized chamber. By doing this, the natural healing process of the body, as well as oxygen delivery to tissues, is enhanced. In conjunction with the healing of tissues, the oxygen stimulates the growth of new blood vessels. This helps improve blood flow to areas with poor circulation. This therapy can increase the white blood cells ability to fight infection, as well as reduce swelling and inflammation. As of July 2021, hyperbaric chambers have been cleared by the Food and Drug Administration (FDA) for the following indications:
- Air and gas bubbles in blood vessels
- Anemia (severe anemia when blood transfusions cannot be used)
- Burns (severe and large burns treated at a specialized burn center)
- Carbon monoxide poisoning
- Crush injury
- Decompression sickness (diving risk)
- Gas gangrene
- Hearing loss (complete hearing loss that occurs suddenly and without any known cause)
- Infection of the skin and bone (severe)
- Radiation injury
- Skin graft flap at risk of tissue death
- Vision loss (when sudden and painless in one eye due to blockage of blood flow)
- Wounds (non-healing, diabetic foot ulcers)
Hyperbaric oxygen therapy is considered safe by the FDA. While complications can occur, they are rare. Some examples of complications are: ear and sinus pain, rupture of the eardrum, temporary vision changes, and lung collapse. There is also the risk of fire due to high concentrations of oxygen.
Hyperbaric chambers can be used for one patient or multiple patients. A monoplace chamber fits one patient. That patient lies on a bed that slides into the chamber, which contains pure, pressurized oxygen. A multiplace chamber can hold two or more patients. The air in the room is pressurized. Each person inhales pure oxygen through a mask or hood.
What Are the Responsibilities of a Hyperbaric Nurse?
A hyperbaric nurse is a specialized registered nurse who is certified to care for patients undergoing hyperbaric oxygen therapy. The Baromedical Nurses Association defines baromedical nursing as the diagnosis and treatment of human response to actual or potential health problems in the altered environment of the hyperbaric chamber. The role has expanded from clinician to include research, education, consulting, surveying, and leadership roles. Updated in 2022, the Baromedical Nurses Association provides nursing guidelines that frame nursing responsibilities in the categories of: risk factors/safety, psychosocial factors, pain, nutrition, condition-specific hyperbaric nursing diagnoses, interventions, and patient/family education. A hyperbaric nurses responsibilities include, but are not limited to:
- Administering hyperbaric oxygen therapy
- Monitoring of patient progress and chamber oxygen levels
- Medication administration
- Assessment of the patient (head-to-toe, vital signs, tympanic membrane assessment, wound assessment, pre- and post-treatment assessments)
- Wound debridement and dressing changes
- Maintaining infection control
- Careful documentation
- Development, implementation, and evaluation of individualized care plans
- Collaboration with multidisciplinary teams
- Equipment management (quality assurance checks and adhering to safety protocol)
- Care management (transfers and discharge planning)
- Patient/family education
While the focus of being a great nurse often lies in the ability to implement effective interventions, patient and family education is sometimes not seen as a vital intervention. Patient and family education is a vital part of nursing in any setting. The education a nurse in a hyperbaric setting can communicate with patients and families includes, but is not limited to:
- Knowledge deficits about the procedure
- Confinement anxiety
- Potential for injury
- Management of expected & potential side effects
- Pain & discomfort management
- Nutrition
- Self-care and wound healing related to hyperbaric oxygen therapy
Where Do Hyperbaric Nurses Work?
Hyperbaric Nurses can be found in various settings:
Hospitals: Hospital-based departments provide care to patients with acute or chronic conditions that require hyperbaric oxygen treatment. This includes medical-surgical, critical care, and emergency department patients. The staffing ratios in these areas are guided by the Undersea and Hyperbaric Medical Society and the National Board of Diving & Hyperbaric Medical Technology.
Outpatient Hyperbaric Centers: These settings offer hyperbaric treatment, usually for wound healing or long-term care. These centers may not have a nurse as a chamber operator; however, there may be a nurse in the role of program director or nurse manager. The Undersea and Hyperbaric Medical Society recommends that office-based hyperbaric oxygen therapy settings maintain the same standards for technicians, nurses, and physicians as their hospital-based counterparts.
Wound Care Clinics: While not all wounds qualify for hyperbaric treatment, hyperbaric nurses can partner with wound care centers or wound care specialists to oversee a hyperbaric treatment as part of a patients overall care plan. In a wound care clinic, the nurse can be a wound care nurse who also has hyperbaric oxygen treatment training. In this case, in addition to hyperbaric nurse certification, the nurse would have a certification in Wound, Ostomy, and Continence Nursing (CWOCN).
Diving Medicine Centers: The very origin of hyperbaric medicine involved calling on nurses to treat divers. As listed before, hyperbaric oxygen therapy treats decompression sickness, which can be caused by rapid drops in water pressure in scuba diving.
How Do I Become a Hyperbaric Nurse?
While hyperbaric nursing originated in Europe in the 1950s, more formal training was not established until the 1960s. In 1985, the Baromedical Nurses Association was started in an effort to recognize hyperbaric nursing as a specialty. This association expanded from the United States to Europe, Asia, South and Central America, and the South Pacific. In 1995, the first Baromedical Nurses Association Certifying Board (BNACB) began to oversee the certification process, which includes RN licensure, Basic Life Support (BLS) certification, designated class hours, and at least one year of hyperbaric experience before completing the exam. In many settings, such as critical care and emergency settings, Advanced Cardiac Life Support (ACLS) certification may also be required. Here is a breakdown of the education required:
Initial Training: Hyperbaric medicine introductory courses are offered with approval by the National Board of Diving & Hyperbaric Medical Technology (NBDHMT) and Undersea & Hyperbaric Medical Society (UHMS). The course is 40 hours.
Certification: There are now three levels of certification:
- Certified Hyperbaric Registered Nurse (CHRN)
- Advanced Certified Hyperbaric Registered Nurse (ACHRN)
- Certified Hyperbaric Registered Nurse Clinician (CHRNC)
Each of the above certifications is eligible to include an administrative certification.
Recognition (-ADM). This applies to a hyperbaric nurse who is no longer involved in direct patient care but holds an administrative role in hyperbaric oxygen treatment. Eligibility criteria include 40-hour training with documented 480 hours of practical clinical experience, a year of hyperbaric nursing work experience, BLS certification, and a letter from the medical director or manager.
Continuing Education: Hyperbaric nurses are required to complete a minimum of 40 hours of continuing education for CHRN certification. For ACHRN and CHRNC certification, a minimum of 60 continuing education hours is required. For all certifications, half of the required hours should be hyperbaric-specific, while the other half can be general hours. The hours must be completed over a four-year period. Of course, this is in addition to completing hours to maintain your nursing licensure. One thing to consider is that if the certification lapses, the hyperbaric nurse will be required to pay fees and re-sit for the certification exam.
After reading this, you may still have questions. You might be interested, but you just do not know where to start. Hyperbaric nursing is a unique route that is of significant value. I encourage you to take a deeper dive into the resources available. This could include contacting the governing bodies for hyperbaric nurses. You may also be interested in contacting hyperbaric oxygen treatment departments to shadow a nurse. Stepping out of the comfort zone of traditional bedside nursing can be intimidating; however, remember that in whatever role you choose, you will make an impact as a nurse. I wish you all the best!
About the Author:
With over 20 years of healthcare experience, Karen has been a registered nurse for 16 years. Her direct patient care background is critical care, with 6 years of experience in the medical intensive care unit. She is Master's-prepared in Nursing Education through Towson University with 14 years of nursing education experience. A portion of her nursing education experience was in the university setting as a clinical instructor, clinical practicum nursing instructor, lecturer, and lab instructor. Her current work and most of her nursing education experience have occurred in the hospital setting, facilitating nursing and interdisciplinary education as a systemwide Nursing Professional Development Specialist II, certified by the American Nurse Credentialing Center (ANCC).
Karen is a published scholarly nursing journal corresponding author, blogger, and continuing education course writer. She is also a certified trainer for Crisis Prevention Institutes Nonviolent Crisis Intervention with Advanced Physical Skills and Johns Hopkins Activity & Mobility Promotion (JH-AMP). In addition, she is a member of the American Nurses Association, the Maryland Nurses Association, the Delaware Organization of Nurse Leaders, the Association of Nursing Professional Development, and the American Association of Critical Care Nurses (AACN).
Karen is an independent contributor to CEUfast's Nursing Blog Program. Please note that the views, thoughts, and opinions expressed in this blog post are solely those of the independent contributor and do not necessarily represent those of CEUfast. This blog post is not medical advice. Always consult with your healthcare provider for any health-related questions or concerns.
If you want to learn more about CEUfast's Nursing Blog Program or would like to submit a blog post for consideration, please visit https://ceufast.com/blog/submissions.